Multiple sclerosis, or MS for short, manifests itself slightly differently in each person—which is why some call it “the disease of a thousand faces.” Arguably the worst manifestation of MS is its chronic progressive form. Unlike the more common relapsing-remitting variant (RRMS), in which sufferers are often symptom-free for months or even years, patients with the primary progressive form of the disease (PPMS) see their condition steadily deteriorate with no remissions.
Poorly insulated neurons die off
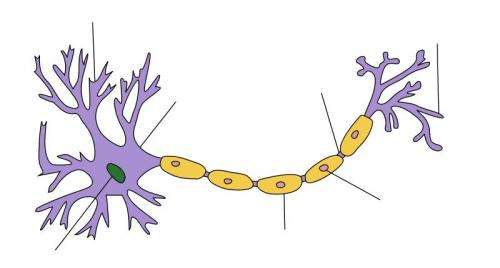
Today’s therapeutic approaches are based on the assumption that the immune system is making a mistake and waging an inappropriate attack on the layer of myelin that surrounds and insulates the nerve cells’ long, cable-like branches called axons. “In progressive MS, neurodegenerative processes steadily multiply and cause more and more neurons in the brain and spinal cord to die,” explains Dr. Alexander Brandt, lead author of the study that has now been published in the journal JAMA Neurology. “However, we still do not know what exactly causes this disease variant.”
Together with Professor Friedemann Paul from the Experimental and Clinical Research Center (ECRC), a joint institution of Charité – Universitätsmedizin Berlin and the Max Delbrück Center for Molecular Medicine in the Helmholtz Association (MDC), as well as eleven colleagues from Berlin, Irvine and Toronto, Brandt now hopes he has shed some more light on the subject. As the team reports in their study, it appears that the simple sugar N-acetylglucosamine, or GlcNAc for short, could play an important role in the development of progressive MS. Inside an organism, GlcNAc and other sugar molecules attach to proteins on the cell surface in the form of chains. This mechanism, which is known as glycosylation, controls various cell functions by forming branched structures from these sugar chains.
The sugar molecule could serve as a biomarker
“We studied 120 subjects from Irvine and were able to show that, in this particularly severe form of the disease, there are significantly lower concentrations of N-acetylglucosamine in the blood serum than there are in healthy people or patients with relapsing-remitting MS,” reports Brandt. At the time of this study, the physician was head of the Translational Neuroimaging laboratory in Paul’s Clinical Neuroimmunology group at Charité. Brandt has since moved to the School of Medicine at the University of California, Irvine (UCI) as an associate professor of neurology, but remains a guest researcher at Charité.
“In another study of 180 patients from Berlin with relapsing-remitting or progressive MS, we also found that low serum levels of GlcNAc are associated with the development of the progressive form of the disease, clinical disability and neurodegeneration,” adds the study’s corresponding author, Professor Michael Demetriou of UC Irvine. “This opens up potential new avenues for identifying, at an early stage, which patients are at higher risk of progressive MS and adjusting their treatment accordingly.”
Human treatment studies now in the pipeline
Back in autumn 2020, Brandt, Demetriou and other researchers working with the then lead author Dr. Michael Sy from UC Irvine published a study in the Journal of Biological Chemistry. They had administered GlcNAc to lactating mice and found that the animals passed on this simple sugar, which incidentally is also contained in human breast milk, to their offspring. This stimulated primary myelination of the neuronal axons in the young animals. “We also observed in the mouse experiments that N-acetylglucosamine activates myelin progenitor cells, thus promoting both primary myelination and the repair of damaged myelin,” says Brandt.
Source: Read Full Article
