(BSS) is an extremely rare, genetic blood-clotting illness marked by large platelet cells, thrombocytopenia, and a protracted bleeding period. Jean-Bernard and Jean-Pierre Soulier documented the first male patient who suffered from recurrent episodes of bleeding throughout his life and died at the age of 28 from a cerebral hemorrhage caused by a bar fight in 1948.
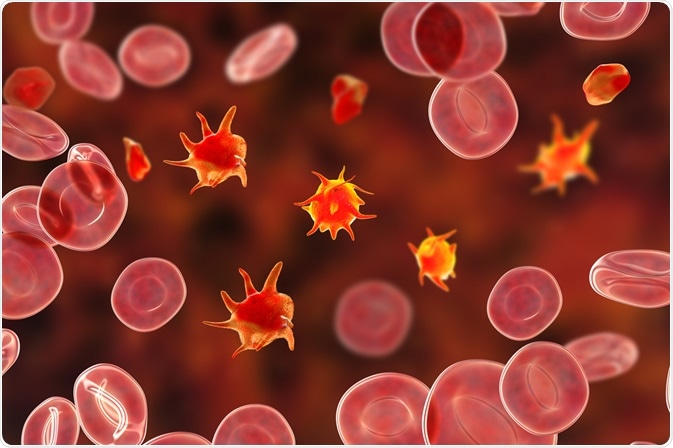
Image Credit: Kateryna Kon/Shutterstock.com
People who are affected tend to bleed a lot and bruise quickly. The majority of people with Bernard-Soulier syndrome have an autosomal recessive genetic pattern. It does, however, have a variety of additional activities in the induction of thrombosis and hemostasis.
Causes and symptoms
BSS is caused by a deficiency in the GPIb-IX-V complex, which is an important platelet receptor complex that binds to the von Willebrand factor (vWF). The tendency to bleed profusely from wounds and other traumas, nosebleeds (epistaxis), and/or an unusually strong menstrual flow in women are all signs of Bernard-Soulier syndrome, which typically appears at birth and last throughout life.
Some babies and children with BSS show no signs or symptoms, and the illness does not manifest itself until adulthood. This disease makes people bruise quickly, and the bruises last a long time. Small or broad regions of small red or purple-colored spots can result from bleeding from very small blood vessels under the skin (subcutaneous) (purpura or petechiae).
Genetics of BSS
GPIb-alpha (GPIBA), GPIB-beta (GPIBB), and GPIX (GP9), which are three of the four subunits that make up the GPIb-IX-V complex, are the cause of BSS. In a study of about 211 families with BSS, roughly 112 mutations were discovered. The mutations were found in the GP1BA (28%) and GP1BB (28%) genes, as well as the GP9 (44%) gene. These mutations can be nonsense, missense, frameshift, deletion, or insertion and are diverse.
Majority of these mutations are autosomal recessive; however, autosomal dominant inheritance has been described in a few cases. Biallelic BSS (bBSS) refers to patients who have mutations in both alleles (autosomal recessive inheritance), while monoallelic BSS (mBSS) refers to patients who have a mutation in only one allele (autosomal dominant inheritance).
With each pregnancy, there is a 25% chance that two carrier parents will both carry the defective gene and, as a result, have an affected child. With each pregnancy, there is a 50% chance of having a child who is a carrier, just like the parents. A child has a 25% chance of inheriting normal genes from both parents. Males and females are equally at risk.
Epidemiology
The disease's prevalence is estimated to be 1 per million. However, the prevalence could be significantly greater than the estimated amount due to under-recognition and misdiagnosis. Because BSS is transmitted through autosomal genes, it affects both men and women.
Bernard-Soulier syndrome is a rare clotting condition that affects both men and women equally. There have been over 200 cases recorded all around the world. Due to its widespread under-recognition, the disease is rarely discovered in the early stages of life, with the average age of diagnosis being 16 years.
Diagnosis
The diagnosis of Bernard-Soulier syndrome is made using a combination of blood tests, microscopic examination, and flow cytometry. Most families are offered molecular genetic testing to determine the gene responsible for the alterations. The platelet count in most BSS patients ranges from 20 to 100 billion per liter. A count as low as 10 x 109/L has been reported. It takes a long time for the bleeding to stop.
Platelet aggregation experiments (also known as light transmission aggregometry) show that ristocetin reduces platelet aggregation, which is not reversed by adding normal plasma. This trait aids in the differentiation of BSS from von Willebrand disease (vWD).
Platelet glycoprotein flow cytometry is a confirming test. It shows a significant decrease in CD42a (GPIX) and CD42b (GPIb-alpha). Flow cytometry is a good test for neonates, babies, and young children because it only requires a tiny amount of blood.
Management and treatment
Patients with BSS should be well taught about the dangers of bleeding. They should have 'alert cards' or wear 'alert wristbands' that clearly state that they have BSS. If they have a bleeding episode, they should be registered with a center that provides emergency treatment 24 hours a day. Patients should also be taught how to keep their teeth clean, avoid high-risk sports (particularly contact sports), and use pressure to relieve epistaxis.
Patients, their families, and their healthcare providers should all be informed about which medications can raise the risk of bleeding (anti-histamines, non-steroidal anti-inflammatory drugs, and certain antibiotics). Foods, beverages, and herbal treatments that can impair platelet function (or number) should be avoided. Patients with BSS, particularly women, can develop iron insufficiency as a result of heavy bleeding and should be regularly monitored for this and given iron supplements if necessary.
Treatment for bleeding episodes involves platelet transfusion, antifibrinolytic therapy, and administration of desmopressin (DDAVP). Because some patients with Bernard-Soulier syndrome acquire antibodies against the GPIb protein, they become resistant (refractory) to platelet transfusions.
To avoid this risk, it is currently suggested that specially selected platelet transfusions (from HLA-matched single donors) be utilized. In the absence of HLA-matched platelets, leucocyte-depleted platelets can be employed (these are platelet transfusions from which contaminating white blood cells-leucocytes- have been removed).
Aspirin and other comparable drugs can harm patients with the syndrome since they affect the blood's capacity to clot (platelet aggregation). Acetaminophen, which is found in drugs such as Tylenol, is thought to be used to treat minor pain. Antifibrinolytic medications (drugs that slow the disintegration of blood clots) are frequently used in minimizing bleeding after a minor surgery (e.g., dental surgery) or in the case of persistent nosebleeds.
Tranexamic acid is the most often used antifibrinolytic medication (also known as epsilon aminocaproic acid). Bernard-Soulier syndrome patients and their families should seek genetic counseling. Symptomatic and supportive treatment is the other option.
References:
- Minkov, M., Zeitlhofer, P., Zoubek, A., Kager, L., Panzer, S., & Haas, O. A. (2021). Novel Compound Heterozygous Mutations in Two Families With Bernard-Soulier Syndrome. Frontiers in pediatrics, 8, 589812. https://doi.org/10.3389/fped.2020.589812
- Almomani MH, Mangla A. Bernard Soulier Syndrome. [Updated 2021 Jul 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557671/
- Bernard-Soulier Syndrome. [online] National Organization for Rare Disorders. Available at: https://rarediseases.org/rare-diseases/bernard-soulier-syndrome/
Further Reading
- All Rare Disease Content
- Teaching old drugs new tricks – drug repurposing for rare diseases
- What is Agnosia?
- What is Ameloblastoma?
- What is Apert Syndrome?
Last Updated: Dec 1, 2021
Source: Read Full Article
