Despite trastuzumab being a game-changing treatment for HER2-positive breast cancers over the past two decades, its success has come with key gaps in the understanding of how, exactly, it works.
That question drove a research team at the Duke Cancer Institute. Publishing in JCI Insight, the researchers used mouse models to track a little-understood mechanism the drug uses to halt tumor growth. Their finding points to potential new ways to enhance that action and thwart drug resistance.
“Trastuzumab is an antibody for the HER2 oncogene and has been a mainstay treatment for the 20 percent of breast cancers fueled by this protein,” said corresponding author Zachary Hartman, Ph.D., assistant professor in the departments of Surgery and Pathology at Duke University School of Medicine.
“It is arguably the most successful antibody therapeutic in treating a solid cancer.”However, there are multiple conflicting explanations for how trastuzumab actually works as an anti-cancer therapeutic,” Hartman said. “A better understanding of how it works could lead to the development of new strategies and more effective antibodies to treat different cancers.”
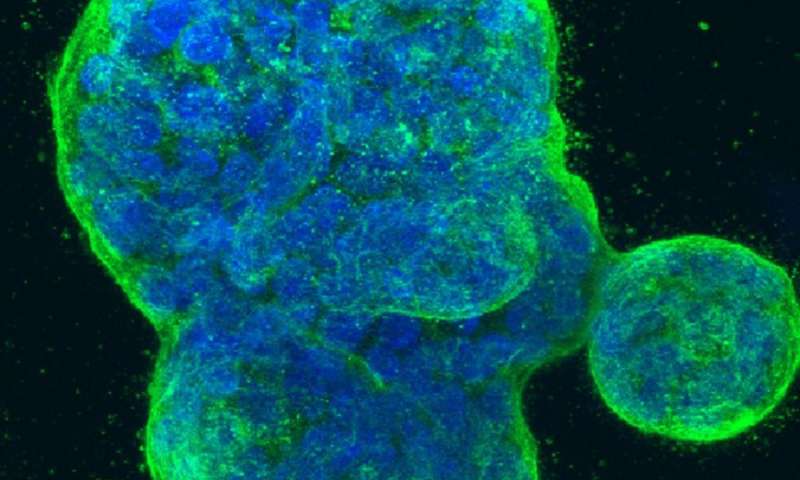
Hartman and colleagues confirmed in mouse experiments and human cell lines that trastuzumab triggers a process called antibody-dependent phagocytosis, which is a way that specific immune cells engulf and eat particles, specifically tumor cells coated with the HER2 antibody.
They also found that by adding another antibody to remove a roadblock in this cell death process, they could strongly improve the drug’s anti-tumor ability. The finding was notable because this roadblock for cell death is driven by the CD47 gene, which is highly expressed in HER2-positive breast cancer patients who have worse outcomes.
Source: Read Full Article
