The current COVID-19 climate has made vaccines, antibodies and immune responses topics of everyday conversation. Now, it isn’t just immunologists who want to know how our bodies respond to re-infections months, years, or sometimes decades after an initial immune response. A new study by Tomohiro Kurosaki at Osaka University shows that this ability requires Bach2, a protein that regulates the expression of genes needed to instruct activated B cells under selection to become memory B cells.
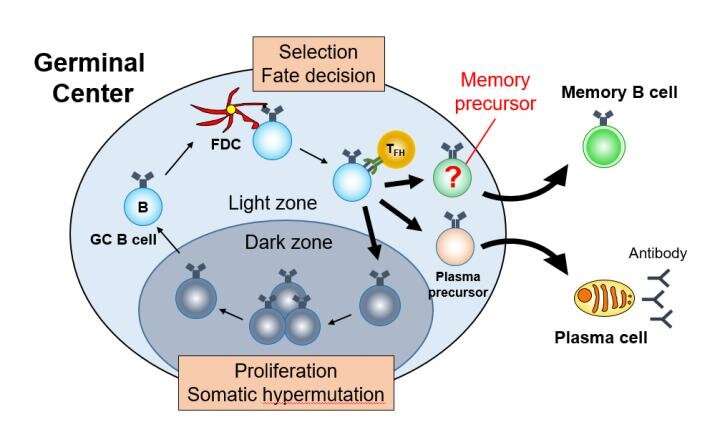
Like most biological processes, immune responses are complicated. They involve numerous types of cells and proteins, performing precise step-by-step processes. And most are as yet unknown. For example, memory B cells are a type of white blood cell created in lymph nodes or spleens during an infection. They stick around for years and allow rapid and strong antibody-related responses to re-infection by the same virus or bacteria. In contrast, plasma cells are much more numerous and help during an initial infection by producing antibodies, although they too can exist for long periods of time in the body. Kurosaki and his team focused their research on understanding what causes activated B cells, called germinal center B cells, to become memory B cells, plasma cells, or to be recycled.
Scientists identify multiple types of B cells by their expression of markers—certain proteins. On the basis of specific markers, the researchers identified a subset of B cells that they determined were prone to become memory B cells, which they called pro-memory B cells. They then examined mice lacking the protein Bach2, a transcription factor required for memory B cell production. These mice are known to be deficient in producing memory B cells. The researchers found that the lack of Bach2 was associated with fewer pro-memory B cells and increased expression of genes related to a protein complex called mTORC1.
Further testing showed the importance of mTORC1. “We ultimately found that mTORC1 signaling was less active in pro-memory B cells than in those that ended up being recycled,” says Kurosaki. Inhibiting mTORC1 activity (in other words, inducing a state of mTORC1 hypometabolism) in the Bach2 knockout mice rescued them, allowing the mice to produce memory B cells. Additionally, in wild-type mice, artificially reducing mTORC1 activity in B cells led to the production of more memory B cells than normal, while increasing its activity had the opposite effect. However, mTORC1 activity alone could not explain everything. Experiments showed that the unique combination of Bach2 expression and reduced mTORC1 activity is necessary to become memory B cells.
Source: Read Full Article
