For the first time, researchers have found a way to predict when a pregnant woman will go into labor by analyzing immune and other biological signals in a blood sample, according to a study from the Stanford University School of Medicine.
The study, which will be published online May 5 in Science Translational Medicine, sheds light on how labor begins, a biological process that until now has been a mystery. The findings lay the groundwork for a clinical blood test that could tell women with healthy, full-term pregnancies how close they are to delivery. Current estimates are imprecise, with anything in a five-week window—from three weeks before to two weeks after the due date—considered a normal delivery time.
The researchers expect their findings to yield a test within the next two to three years that doctors can use to predict labor onset in healthy pregnancies. The method narrows the predicted delivery time to a two-week window, and the researchers expect it will become even more precise as the technique is refined.
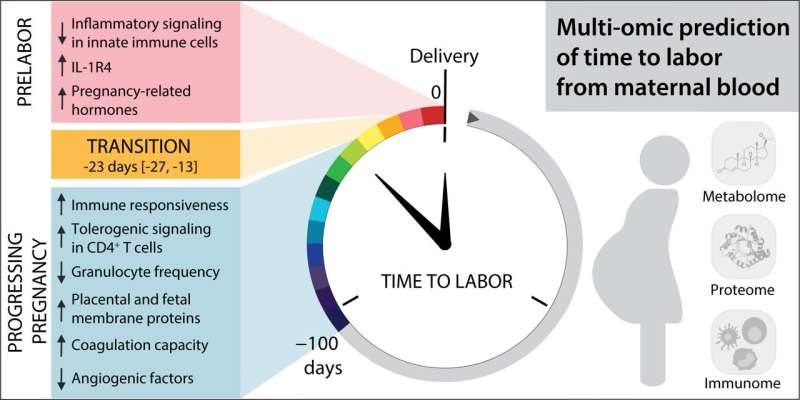
“We found a transition from ‘progressing pregnancy’ to a ‘pre-labor’ phase that happens two to four weeks before the mom goes into labor,” said Ina Stelzer, Ph.D., the study’s lead author and a postdoctoral scholar in anesthesiology, perioperative and pain medicine at Stanford. “We’ve identified a novel way to use the maternal blood to predict when a mother will go into labor. This prediction is independent from the duration of pregnancy.”
The shift from ongoing pregnancy to the pre-labor phase was detected both in women who had full-term pregnancies and in women who delivered prematurely. The change to pre-labor maternal biology is characterized by changes in levels of steroid hormones, factors that control blood vessel growth and blood coagulation, and immune regulatory signals, the study found.
“The mom’s body and physiology start to change about three weeks before the actual onset of labor,” said co-author Virginia Winn, MD, Ph.D., associate professor of obstetrics and gynecology at Stanford. “It’s not a single switch; there’s this preparation that the body has to go through.”
Getting mother and baby ready for birth
Clinicians currently estimate a woman’s due date by counting 40 weeks from the first day of her last menstrual period and taking into account ultrasound data about the baby’s size.
“Clinicians are good at estimating gestational age, which measures the development of the fetus. But there is a disconnect between this timing and when labor starts, because whether the baby is ready is only one factor in the onset of labor,” said Brice Gaudilliere, MD, Ph.D., the study’s senior author and associate professor of anesthesiology, perioperative and pain medicine. “The other part of the equation is the mother.”
The study is one of many findings about the biology of pregnancy to come out of Stanford’s Prematurity Research Center.
Although women deliver around 40 weeks of pregnancy on average, going into labor at anywhere from 37 to 42 weeks’ gestational age is considered normal. More precise prediction of when the baby will arrive could be helpful, for both planning and medical reasons. For instance, being able to test whether a woman with preterm contractions is in the pre-labor phase could help doctors decide whether to administer steroids, which mature the fetus’s lungs before birth.
The study followed 63 women through the last 100 days of their pregnancies. They gave blood samples for analysis two to three times before delivery. All of them went into labor spontaneously, meaning none were artificially induced.
Each blood sample was analyzed for 7,142 metabolic, protein and single-cell immune features. The data was plotted against the number of days before labor that each blood sample had been taken, ensuring that the analysis would be sensitive to signals of impending labor, as opposed to signals tied primarily to pregnancy duration or the baby’s growth. The researchers identified, via mathematical modeling, which features in the blood best predicted labor onset.
Fifty-eight of the women gave birth after full-term pregnancies, meaning the baby did not arrive more than three weeks before the due date, and five gave birth after spontaneous preterm labor.
As they moved into the pre-labor phase, the women’s blood showed surges in steroid hormones such as progesterone and cortisol, confirming prior findings about the biology of late pregnancy. The blood also showed decreasing levels of factors that help blood-vessel formation, likely a first step toward weakening the connection between the placenta and uterus, as well as increasing levels of factors needed for blood coagulation, which help prevent blood loss after delivery. Some placental proteins surged as well.
The study also found a fine-tuning of immune responses in the shift to labor preparation. The top predictive feature in the model was a regulatory immune protein, IL-1R4, that inhibits an inflammatory molecule called IL-33, the researchers said.
“We were really interested in and excited about the finding that IL-33 seems to play a role in pregnancy and impending labor,” Stelzer said. Near the end of pregnancy, placental material and fetal cells reach the mom’s blood, potentially causing an immune response. The body needs to carefully tailor the amount of inflammation that will occur during labor, Stelzer said.
“The hypothesis has been that labor is an inflammatory reaction, and yes, there are signs of that, but we also found that aspects of this inflammation are toned down before labor starts, which we think may prepare the mother’s immune system for the next phase, when the baby is born and healing and immune resolution begins,” Gaudilliere said. “It needs to be a regulated process.”
The next steps in the research are to validate the findings in more pregnant women and to narrow the number of biological markers needed to predict labor onset, Stelzer said, adding that the team has already made progress on the latter.
Source: Read Full Article
