In patients with spinal cord injuries, a medical emergency known as autonomic dysreflexia can occur and have potentially life-threatening consequences. Autonomic dysreflexia, also known as autonomic hyperreflexia, occurs when there is pain or discomfort below the spinal cord injury that leads to elevated blood pressure levels, which can in turn cause stroke, seizure, organ damage, or death.
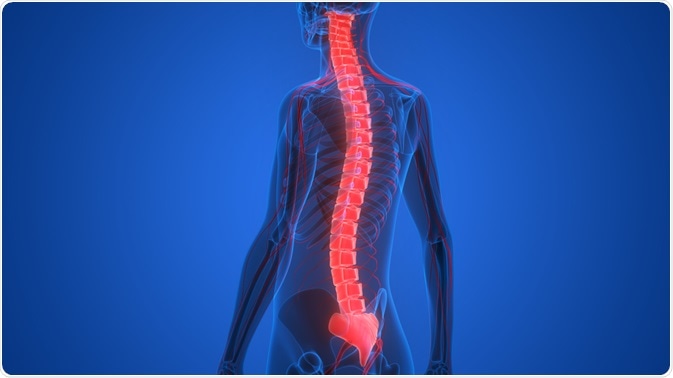
Image Credit: Magic mine/Shutterstock.com
How does autonomic dysreflexia occur?
Autonomic dysreflexia only occurs in those who have a spinal cord injury at the sixth thoracic vertebrae or higher, although it can more rarely occur in those with injuries to the seventh to tenth vertebrae.
If the spinal cord injury is at the tenth thoracic vertebrae, there is no risk of autonomic dysreflexia. It is estimated that autonomic dysreflexia occurs in around 49% of those with spinal cord injuries at the sixth thoracic vertebrae or higher.
Autonomic dysreflexia means that the autonomic nervous system is overactive. It occurs when signals of pain or discomfort cannot reach their intended destination. The spinal cord injury prevents messages of pain from being communicated to the brain and instead causes the blood pressure to increase dangerously.
In a healthy body, the vessels around a site of injury could be signaled to dilate to reduce the danger of high blood pressure. However, in autonomic dysreflexia, this signal is blocked by the spinal cord injury and the rise can thus become dangerous. Autonomic dysreflexia constitutes this rise in blood pressure, which can be as little as 20 mm Hg above normal in adults but can still have fatal consequences.
While an increase in 20 mm Hg can still mean the blood pressure is within a healthy person’s normal range, the effects on the body are significant. A sudden increase in blood pressure can mean the veins and arteries are not acclimatized to that level of pressure and can burst.
Causes and signs of autonomic dysreflexia
The most common cause of autonomic dysreflexia is bladder issues. This can include benign problems, such as the bladder being too full, or more serious problems, such as urinary tract infections or kidney stones. This can especially be the case in patients with catheters, as bladder discomfort can thus be caused by clogged catheters and full or defective catheter bags. The bladder discomfort can also stem from medical exams, such as urodynamics.
Discomfort leading to autonomic dysreflexia can also be caused by bowel issues. The issues can include constipation, hemorrhoids, gas or bloating, and infection of the bowels. Occasionally, the discomfort can stem from medical procedures.
A third major cause of autonomic dysreflexia are skin issues. These can be small, such as insect bites and blisters, or more widespread afflictions, such as sunburns. Other issues include pressure sores, ingrown toenails, constrictive clothing, hard objects adjacent to the skin, and otherwise awkward positions that can cause constriction to different body parts.
While these are three major sources of discomfort that lead to autonomic dysreflexia, any discomfort below the level of the injury can cause autonomic dysreflexia. Other sources of discomfort include various abdominal problems such as gallstones and stomach ulcers, reproductive problems such as menstruation and pregnancy or delivery, blood clots, heterotopic ossification, broken bones, muscle tightness, or temperature fluctuations.
Symptoms of autonomic dysreflexia can vary between people. The main sign of autonomic dysreflexia is an increase in systolic and diastolic blood pressure. Some of the other common signs include headaches, flushed face, sweating above the location of the spinal cord injury, and prickly skin below the level of the injury. Other symptoms include a stuffy nose, nausea, and a pulse below 60 beats per minute.
Management and treatment
Management of autonomic dysreflexia focuses largely on altering habits and responding to the symptoms, with medications generally avoided unless the original discomfort cannot be identified or removed. Sometimes approaches aim to target the symptoms of autonomic dysreflexia, however, there can be complications to this.
For example, high blood pressure can be treated in otherwise healthy patients with baroreceptor induced vasodilation. However, in patients with spinal cord injuries, this is often not helpful.
Acute treatment of acute dysreflexia involves correcting posture to prevent further increases in blood pressure. Therefore, the patient should sit upright with lowered legs, if possible. This should, preferably, be followed by identification of the cause. This could include, for example, checking for urinary problems or other sources of discomfort.
More long term treatment options for autonomic dysreflexia are varied. Many focus on reducing the original discomforts that trigger it in the first place, but others also focus on lowering general hypertension using medication. A commonly used one is glyceryl trinitrate.
Sources
- Christopher and Dana Reeve Foundation. 2020. Autonomic Dysreflexia. [online] Available at: <https://www.christopherreeve.org/living-with-paralysis/health/secondary-conditions/autonomic-dysreflexia> [Accessed 18 August 2020].
- Karlsson, A., 1999. Autonomic dysreflexia. Spinal Cord, 37(6), pp. 383-391.
- Craig Hospital. 2015. Autonomic Dysreflexia. [online] Available at: <https://craighospital.org/resources/autonomic-dysreflexia> [Accessed 18 August 2020].
Last Updated: Aug 19, 2020

Written by
Sara Ryding
Sara is a passionate life sciences writer who specializes in zoology and ornithology. She is currently completing a Ph.D. at Deakin University in Australia which focuses on how the beaks of birds change with global warming.
Source: Read Full Article
