A new trial has shown a sizeable and significant benefit of endovascular thrombectomy in acute ischemic stroke patients with a large vessel occlusion and an established large infarct identified with just simple imaging techniques, which should lead to many more patients able to be considered for this treatment.
The TENSION trial, conducted in patients with severe strokes who would normally have an extremely poor prognosis, showed that thrombectomy resulted in an 18% absolute increase in the number of patients able to walk independently at 90 days and an 11% reduction in mortality at 90 days compared to medical therapy alone. There was a consistent benefit of thrombectomy across all categories of outcome, sensitivity analyses, and subgroups.
In addition, there were no safety concerns or increase in severe or symptomatic intracranial hemorrhage with thrombectomy.
“This pragmatic approach based on visual assessment of non-contrast CT yielded similar benefit to trials with more complicated and time-consuming imaging approaches and shows that thrombectomy should be considered in patients with stroke from large vessel occlusion and an already established large infarct,” concluded senior investigator Götz Thomalla, MD, University Hospital Hamburg-Eppendorf, Germany.
Thomalla presented the TENSION trial this week at the World Stroke Conference 2023 being held in Toronto, Canada, where it was enthusiastically received. In fact, the audience broke into applause when the main results were shown. It was also simultaneously published online in The Lancet.
As background, Thomalla explained that endovascular thrombectomy has been shown to be highly effective in improving outcomes in patients with acute ischemic stroke due to large vessel occlusion and who have a small or moderate infarct size. Patients with larger brain infarcts are frequently excluded from endovascular thrombectomy, even though they constitute up to 25% of ischemic strokes due to large vessel occlusion in routine clinical practice.
Three recent trials have provided evidence of benefit for endovascular therapy in patients with a large infarct. But Thomalla noted that these trials — RESCUE-JAPAN LIMIT, SELECT-2 and ANGEL-ASPECT — have limited generalizability because they included selected populations in Asia and they identified patients for enrollment with the use of advanced imaging (perfusion CT or MRI), whereas in most centers, stroke imaging in clinical practice relies on unenhanced CT or CT angiography.
The current TENSION trial was conducted to assess whether endovascular thrombectomy improves functional outcome in stroke patients with large vessel occlusion and a large infarct based on clinical standard imaging.
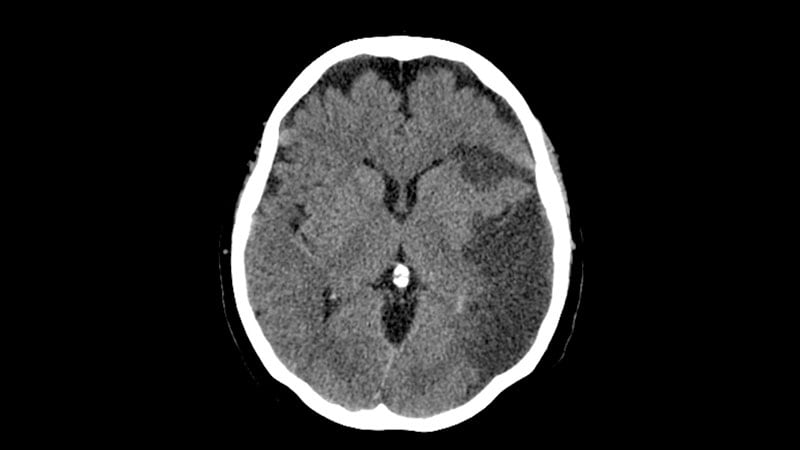
The investigator-initiated trial planned to enroll 665 patients from nine countries (eight European countries and Canada) with large vessel occlusion and an extended infarct (ASPECTS 3-5) on visual assessment of non-contrast CT or MRI who were within 12 hours of stroke onset. Patients were randomly assigned to receive endovascular thrombectomy plus medical management or medical management alone (control).
Baseline characteristics showed that a median National Institutes of Health Stroke Scale (NIHSS) score of 19, which Thomalla said showed a “really severely affected population” reflecting the large vessel occlusion and large infarct size. Thrombolysis was given in about one third of patients. In more than 80% of patients, standard CT was used as the imaging method.
The trial was stopped early because of efficacy at the first interim analysis after the enrollment of 253 patients.
Results showed that at 90 days, endovascular thrombectomy was associated with a shift in the distribution of scores on the modified Rankin Scale (mRS) toward a better outcome (adjusted common odds ratio, 2.58, 95% CI, 1.60 – 4.15; P = .0001). The median mRS score in the thrombectomy group was 4 vs 6 in the control group.
There was also significant benefit in the dichotomous endpoints of functional independence — mRS scores of 0-2 or 0-3.
In the secondary outcome analysis, 17% of patients in the endovascular thrombectomy group achieved a score of 0-2 on the mRS at 90 days as compared with just 2% in the medical treatment group (adjusted OR, 7.16; P = .0016).
And 31% of patients in the endovascular thrombectomy group had a score of 0-3 on the mRS at 90 days vs 13% of those in the medical treatment group (adjusted OR, 2.84; P = .0018).
Thomalla highlighted the very low number of patients achieving the 0-2 levels of functional independence (2%) in the control group, which he said, “shows how severely affected these patients are and how poor the prognosis is with medical treatment alone.”
Death from any cause at 90 days occurred in 40% of those who received endovascular thrombectomy vs 51% of those in the medical treatment alone group, an absolute reduction in mortality of 11% (hazard ratio, 0.67; P = .038).
“In this population, thrombectomy really is saving lives. In this study, it saved the life of 1 patient in every 9 that were treated,” Thomalla commented.
Thrombectomy was also associated with a significant reduction of death or dependency (modified Rankin Scale 4-6) at 90 days, with this endpoint occurring in 69% of patients in the thrombectomy group vs 87% of those receiving medical treatment only (adjusted OR, 0.34; P = .0011).
There was no difference in parenchymal hemorrhage rate between the two groups, with no increase in parenchymal hemorrhage type 2, symptomatic intracranial hemorrhage, or fatal hemorrhage with thrombectomy, which Thomalla described as “remarkable.”
Symptomatic intracranial hemorrhage occurred in seven (6%) patients with thrombectomy and in six (5%) with medical treatment alone.
Thomalla added: “This is very reassuring as this is one of the things that makes clinicians reluctant to do thrombectomy in these patients with large infarcts, because they are afraid of hemorrhage into these large lesions.”
Commenting on the study for theheart.org | Medscape Cardiology, Thanh Nguyen, MD, professor of neurology, neurosurgery, and radiology at Boston University School of Medicine, said the TENSION trial was another pivotal trial adding to the evidence in favor of treating patients with large ischemic core.
“It is important because, similar to the TESLA trial, the study has liberal inclusion criteria in allowing the brain parenchyma selection of patients based on CT alone (over 80% of patients were selected with CT in TENSION). This permits generalizability of the study results to centers that do not have readily available access to MRI or CT perfusion capability, and also will likely improve workflow times,” Nguyen noted.
“If patients with low ASPECTS (3 to 5) on CT are good enough for CT selection for thrombectomy out to the 12-hour window, then this implies that patients with good ASPECTS (6 to 10) on CT alone are also deserving for thrombectomy without need for further advanced imaging (which is currently considered required or necessary in most guidelines),” she added.
Meta-analysis Needed?
In an accompanying editorial, Diederik Dippel, MD, and Bob Roozenbeek, MD, from Erasmus MC University Medical Center, Rotterdam, the Netherlands, explain that in acute ischemic stroke patients presenting after 6 hours from symptom onset, CT perfusion is often used to compare contrast flow in the affected area with the flow in the healthy hemisphere.
In this way, CT perfusion is supposed to distinguish hypoperfused but viable tissue (the ischemic penumbra) from the ischemic core and can be used to help select patients who might benefit from the treatment, even after more than 6 hours since stroke onset.
But they say that use of CT perfusion requires expertise, special software, and, for each patient, time. “Time is highly relevant because ‘time is brain’ in an ischemic stroke,” they add.
Dippel and Roozenbeek note that the TENSION trial is the first randomized trial of endovascular thrombectomy in patients with large infarctions that based patient selection on non-contrast CT and CT angiography only, without CT perfusion.
They point out that the TENSION trial included patients only if the stroke onset or time last seen well was less than 12 hours before random assignment, criteria which limits generalizability, because, in many countries, at least a third of patients with ischemic stroke present between 12 and 24 hours from onset.
They also note that trials that are stopped early for efficacy, such as TENSION, are small, and typically report large effects that are much less likely to occur than when the trial is carried out until the end. Thus, results of these trials should be considered carefully, and confirmation will be needed.
The authors note that three other large-core trials that used more complex imaging have been reported previously — and results from at least two more large-core trials are expected.
They urge the investigators to combine their data in individual patient-data meta-analyses, which, they say, “will help us to define which and how many more patients might benefit from simple selection for this highly effective treatment for ischemic stroke.”
The TENSION trial was supported by the EU Horizon 2020 research and innovation program.
World Stroke Conference 2023. Presented October 11, 2023.
The Lancet. Published online October 11, 2023. Full text, Editorial
For more from theheart.org | Medscape Cardiology, join us on X (formerly Twitter) and Facebook
Source: Read Full Article