TOPLINE:
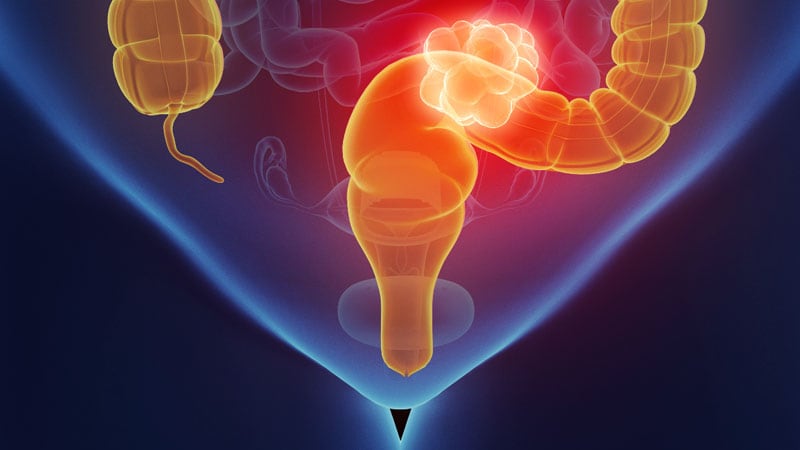
Proctectomy and other surgeries are falling out of favor to treat stage II and III rectal cancer in the United States.
METHODOLOGY:
-
The National Comprehensive Cancer Network endorses watchful waiting, instead of surgery, when patients with rectal cancer have a complete clinical response to neoadjuvant therapy, but it’s unclear how often patients and providers opt for this organ preservation approach.
-
To find out, investigators reviewed 175,545 adults in the National Cancer Database treated for rectal adenocarcinoma from 2006 to 2020.
-
The research team assessed changes in the proportion of patients who were treated with chemotherapy and/or radiation without tumor resection, transanal local excision, or removal of the rectum.
-
Patients had a mean age of 63 years, 39.7% were women, 17.4% had stage 1 disease, 24.7% had stage 2A-C disease, and 32.1% had stage 3A-C tumors; tumor stage was unknown in just over a quarter of patients.
TAKEAWAY:
-
The absolute annual proportion of organ preservation increased by more than 50% from 18.4% in 2006 to 28.2% in 2020.
-
In that time frame, organ preservation increased from 19.5% to 32.5% — a percent increase of about 67% — for patients with stage 2A-C disease, 16.2% to 29.1% — a percent increase of about 80% — for patients with stage 3A-C disease, and 16.5% to 26.6% — a percent increase of about 60% — for those with unknown stages.
-
However, the rate of proctectomies increased by 6.1 percentage points, or by about 30%, among patients with stage I rectal cancer — from 20.3% to 26.4%.
-
Among patients who did have surgery, the proportion who had complete pathologic responses to neoadjuvant therapy nearly tripled, increasing from 6.5% to 18.8%.
IN PRACTICE:
“This case series shows that rectal cancer is increasingly being managed medically, especially among patients whose treatment historically relied on proctectomy,” the authors conclude. However, protocols to standardize the approach are lacking, which is why “establishing quality standards for organ preservation is a pressing issue that should involve all relevant stakeholders, including patients.”
SOURCE:
The study, led by Anthony Loria, MD, MSCI, of the University of Rochester, New York, was published online November 9 in JAMA Oncology.
LIMITATIONS:
The percentage of people who needed surgery for recurrence, patient and facility factors associated with organ preservation, and overall survival outcomes were not addressed.
DISCLOSURES:
No external funding was reported, and the investigators reported no relevant financial relationships.
M. Alexander Otto is a physician assistant with a master’s degree in medical science and a journalism degree from Newhouse. He is an award-winning medical journalist who worked for several major news outlets before joining Medscape. Alex is also an MIT Knight Science Journalism fellow. Email: [email protected]
Source: Read Full Article