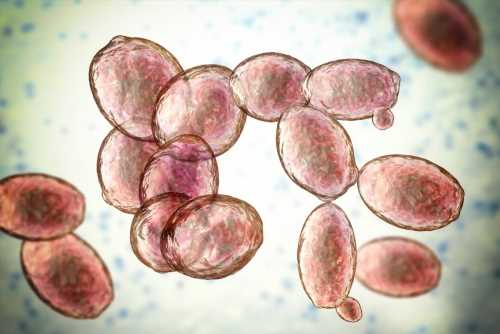
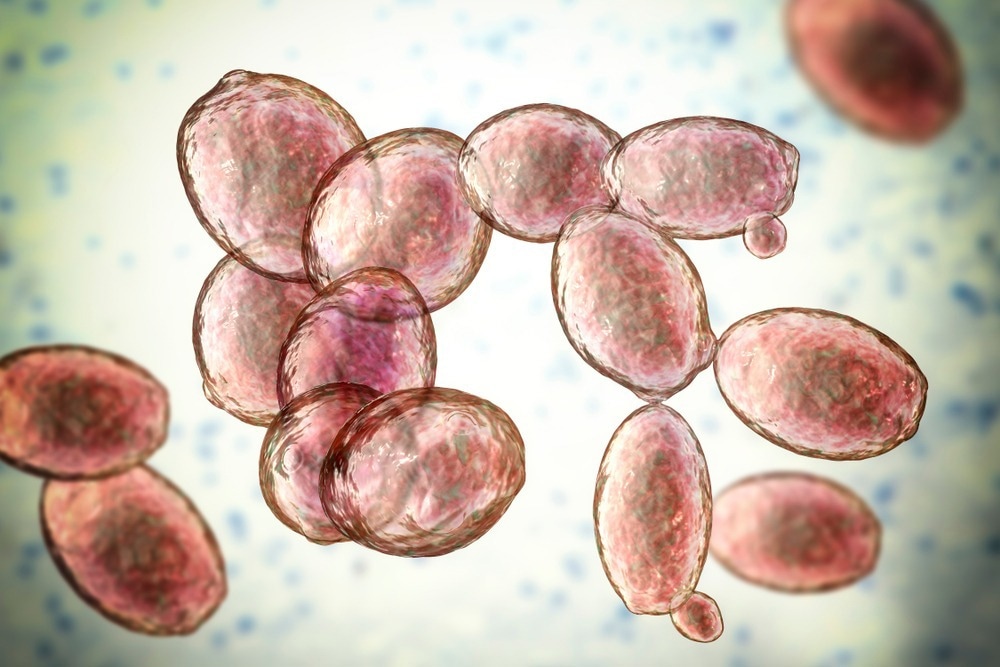
In a recent study published in Tropical Medicine and Infectious Disease, a team of researchers from Brazil presented a fatal case of a patient developing Saccharomyces cerevisiae infection and succumbing to septic shock after contracting and recovering from a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.
Background
Immunology eBook
While the mortality rates associated with the coronavirus disease 2019 (COVID-19) were extremely high worldwide, many patients hospitalized or admitted to intensive care units also faced the additional complication of bacterial and fungal co-infections. Furthermore, the immune dysregulation caused by COVID-19 exacerbated the risk of opportunistic bacterial and fungal infections.
Various studies have reported co-infections with yeasts such as Candida species, S. cerevisiae, and Cryptococcus neoformans, molds such as Aspergillus, Rhizopus, and Mucor, and dimorphic fungi such as Paracoccidioides species and Histoplasma capsulatum in severe COVID-19 patients.
A recent increase in Saccharomyces infections has been observed among critically ill patients, which is thought to be linked to the probiotic dietary supplements given to ease diarrhea caused by antibiotics. Given the increasing risk of Saccharomyces infections among immunocompromised and critically ill patients, its virulence needs further investigation.
About the study
In the present study, the researchers reported a case study of a 75-year-old woman with other health complications who was scheduled for a left foot amputation after being admitted for an arterial ulcer and whose condition rapidly declined after being symptomatically treated for a SARS-CoV-2 infection. Although the patient died due to septic shock four days after hospitalization, blood samples were collected and cultured, and yeast-like organisms were detected.
The yeast-like organisms, identified to be S. cerevisiae were used to evaluate whether the biofilm-forming and planktonic cells were susceptible to standard antifungal medications, whether fungal virulence was associated with the production of siderophores, hemolysins, and hydrolytic enzymes, whether these cells could grow in various nutrient sources, and whether they could infect the Tenebrio molitor larvae or mealworm larvae in vivo.
Results
The case report indicated that the patient had a history of smoking, systemic arterial hypertension, and stroke with aphasia. Positive SARS-CoV-2 polymerase chain reaction (PCR) tests 30 and 10 days before hospital admission indicated COVID-19, which was treated at home symptomatically.
However, the patient’s condition worsened rapidly with metabolic acidosis, bradycardia, hypotension, leukocytosis, high levels of C-reactive protein, and disorientation. She was treated with intravenous antimicrobials and monitored for atrial fibrillation. Four days after hospitalization, the patient succumbed to septic shock, and blood cultures of samples taken six hours before her death revealed yeast-like organisms that were later identified as S. cerevisiae.
The identification of the yeast was based on metabolic, enzymatic, and carbohydrate assimilation profiles based on a yeast card, as well as the amplification of ITS1-5.8S-ITS2 gene sequences, which were matched to those of Saccharomyces in the GenBank database.
Five antifungals — amphotericin B, caspofungin, fluconazole, 5-flucytosine, and voriconazole — were tested against the strain, and for all five, the strain displayed low minimal inhibitory concentrations, indicating that it was susceptible. However, the fungal strain was able to produce biofilms and virulence factors, including extracellular bioactive molecules such as aspartic peptidase, catalase, esterase, hemolysin, phospholipase, phytase, and siderophore.
While the antifungals were effective against planktonic cells, they were not able to suppress mature biofilms in terms of viability and biomass parameters. Experiments with Tenebrio molitor also showed that the isolated S. cerevisiae strain caused the death of the larvae, and the mortality rate increased based on fungal inoculum and the suppression of the larval immunity using corticosteroids.
The authors also discussed another report of a COVID-19 patient developing S. cerevisiae infection after being prescribed Saccharomyces supplements to alleviate diarrhea caused by the antibiotics. While treatment with fluconazole was successful against the fungal infection, the patient succumbed to pulmonary infection and other COVID-19 secondary complications.
The results indicated that classical antifungals are effective in treating S. cerevisiae infections, with the exception of fluconazole, which has varying susceptibility profiles. Furthermore, the reduced effectivity of the antifungals against biofilms presents an additional challenge in treating opportunistic fungal infections in critically ill patients.
Conclusions
The case study indicated that the patient succumbed to septic shock after contracting an S. cerevisiae infection post-SARS-CoV-2 infection. The isolated Saccharomyces cerevisiae strain was seen to be susceptible to classical antifungals in the planktonic cell state but not as biofilms.
Furthermore, the production of extracellular bioactive molecules indicated virulence. Given the use of S. cerevisiae as dietary supplements during antibiotic treatment, the authors believe that S. cerevisiae should be recognized as an opportunistic pathogen.
- Ramos, L. et al. (2023) "SARS-CoV-2 Post-Infection and Sepsis by Saccharomyces cerevisiae: A Fatal Case Report—Focus on Fungal Susceptibility and Potential Virulence Attributes", Tropical Medicine and Infectious Disease, 8(2), p. 99. doi: 10.3390/tropicalmed8020099. https://www.mdpi.com/2414-6366/8/2/99
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Amputation, Antibiotic, Antifungal, Aphasia, Atrial Fibrillation, Biofilms, Blood, Bradycardia, Candida, Carbohydrate, Cell, Coronavirus, covid-19, C-Reactive Protein, Diarrhea, Foot, Fungal Infection, fungi, Gene, Hospital, Hypotension, immunity, in vivo, Intensive Care, Medicine, Mortality, Pathogen, Polymerase, Polymerase Chain Reaction, Probiotic, Protein, Respiratory, S. cerevisiae, Saccharomyces Cerevisiae, SARS, SARS-CoV-2, Sepsis, Septic Shock, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Smoking, Stroke, Supplements, Syndrome, Ulcer, Voriconazole, Yeast
.jpg)
Written by
Dr. Chinta Sidharthan
Chinta Sidharthan is a writer based in Bangalore, India. Her academic background is in evolutionary biology and genetics, and she has extensive experience in scientific research, teaching, science writing, and herpetology. Chinta holds a Ph.D. in evolutionary biology from the Indian Institute of Science and is passionate about science education, writing, animals, wildlife, and conservation. For her doctoral research, she explored the origins and diversification of blindsnakes in India, as a part of which she did extensive fieldwork in the jungles of southern India. She has received the Canadian Governor General’s bronze medal and Bangalore University gold medal for academic excellence and published her research in high-impact journals.
Source: Read Full Article