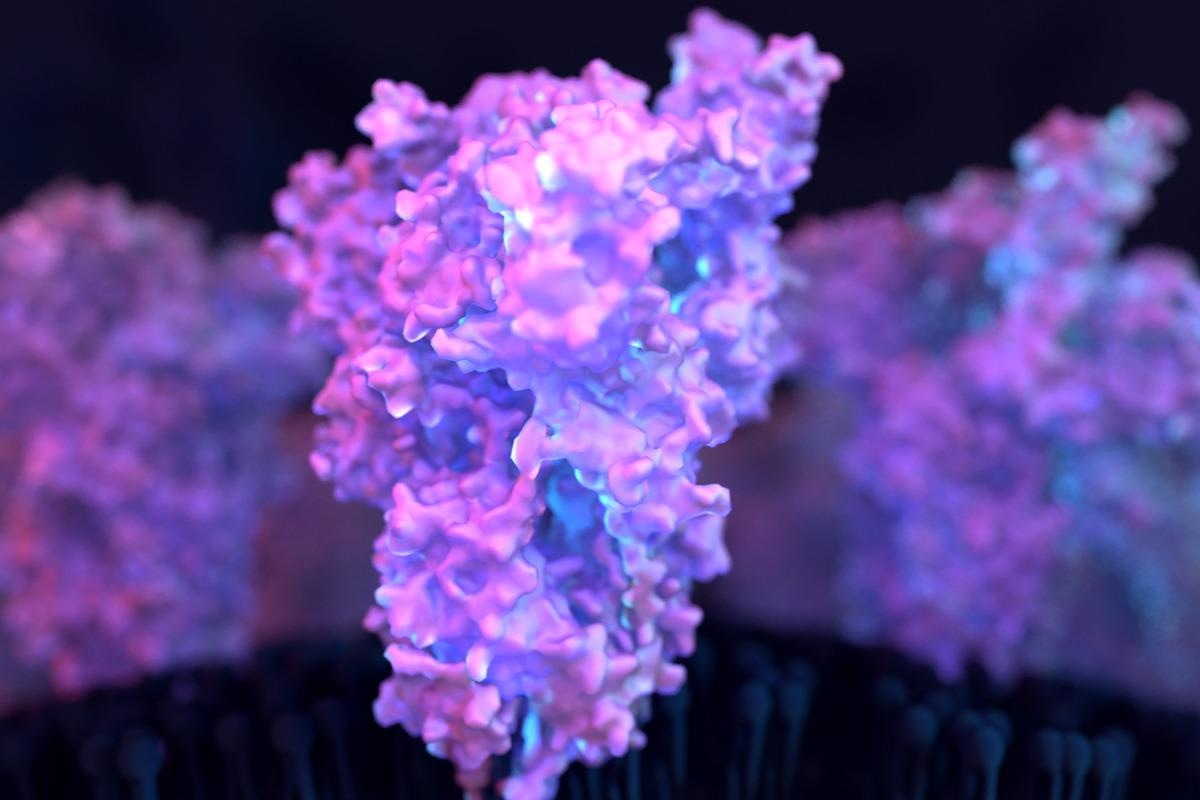
A recent study published in PLOS ONE analyzed the polymorphisms in the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike (S) proteins' S1/S2 subunits.
Background
The SARS-CoV-2's S protein mediates the host entry of the virus. The S protein interacts with the host angiotensin-converting enzyme 2 (ACE2) receptor through its S1 subunit. Fusion between the viral membrane and the host cell membrane is facilitated by the S2 component of the S protein, enabling the release of the viral genome into the cytoplasm of the host cell.
For optimal entrance to lung cells, the S protein needs cleavage at the S1/S2 site positioned inside the extended loop at the S1 and S2 subunit interfaces. Of note, the characteristic feature of the S1/S2 cleavage site is a multibasic motif. The cellular protease furin cleaves S proteins at the S1/S2 site, and robust cleavage at this location may be essential for SARS-CoV-2's host immune evasion. It is the driving factor of SARS-CoV-2 transmissibility and pathogenicity.
Many recently emerged SARS-CoV-2 variants exhibit mutations in their S proteins' surface units. Hence, it is essential to uncover the cellular and viral characteristics that enhance viral propagation in the host's upper respiratory tract, which leads to enrichment of SARS-CoV-2 transmission.
About the study
In the current work, the researchers determined if the ten commonly-occurring mutations inside the SARS-CoV-2 S proteins' extended loop containing the S1/S2 cleavage site regulate viral pathogenicity and cell tropism. The ten mutations analyzed were A684S, A684V, A684T, Q675R, A688V, P681H, V687L, S686G, Q677H, and P681L. The team also assessed whether these mutations influenced the S protein function and processing.
Cell culture was conducted using human embryonic kidney 293T (HEK293T) cells, Vero (African green monkey kidney) cells, Calu-3 (human lung) cells, Caco-2 (colon epithelial) cells, and A549 (human lung) cells. The plasmids utilized for the experiments included pCAGGS-vesicular stomatitis virus G (pCAGGS-VSV-G), pCAGGS-DsRed, pCG1-SARS-2-SΔ18, and pCG1-ACE2. Cell-cell fusion assay was conducted using the HEK293T cells. VSV pseudoparticles (VSVpp) were generated by the authors using HEK293T cells.
Findings and discussions
The results of prediction analysis regarding the chances of cleavage of the SARS-CoV-2 S protein by proprotein convertases like furin demonstrated no variation among the SARS-CoV-2 mutant and wildtype (WT) sequences. The lone exception was an engineered mutant S protein with a single alanine residue (ΔS1/S2) instead of the multibasic cleavage motif.
All SARS-CoV-2 S protein mutants were substantially integrated into the VSVpp. No relevant variations were observed in the S protein integration among the mutant and WT sequences. A single exception was the A684S mutant, which exhibited slightly higher VSVpp incorporation. As predicted, the VSVpp primarily included S protein cleaved at the S1/S2 site, as demonstrated by a strong, approximately 90 kDa band correlating with the S2 subunit.
Furthermore, significantly less pronounced bands belonging to the uncleaved S protein (S0) were detected. Multiple tests measuring the S2 and S0 signals demonstrated that none of the ten mutations evaluated enhanced S protein cleavage at the S1/S2 region. On the contrary, five mutations: P681L, P681H, A684S, V687L, and S686G, were discovered to induce a substantial decline in S protein cleavage relative to the WT strain. These data indicate that numerous naturally occurring polymorphisms can influence the efficiency of S protein cleavage.
None of the evaluated mutant S proteins demonstrated a lower capacity to interact with the host ACE2 receptor than the WT S protein. The majority of the mutant S proteins showed no relevant differences in ACE2 binding ability. The lone exception was S686G mutant, which induced a moderate yet statistically meaningful elevation in ACE2 binding. This suggests that the mutations investigated in the present study did not impair ACE2 binding, and one somewhat enhanced it.
The 10 S protein mutations studied displayed the same efficiency in cell-cell fusion involving ACE2-transmembrane protease serine 2 (TMPRSS2) or ACE2 as the SARS-COV-2 WT S proteins. All S protein mutations facilitated viral entrance into the examined cell lines but with varying degrees of efficiency relative to the WT S proteins. Of the ten S protein mutants analyzed, just the S686G mutation demonstrated varied and cell line-dependent viral-cell entry characteristics relative to the WT S protein. The S686G mutant lowered viral entry in the Caco-2 and Calu-3 cells, whereas it enriched the A549-ACE2 and Vero cells' viral entry.
Targeted expression of Calu-3 cells stably expressing cathepsin L (CTSL) heightened the cell entry of the S686G mutant. Similarly, the Calu-3 cell entry of mutants without S1/S2 sites was dramatically enhanced following directed CTSL expression compared to WT S protein. These findings imply that CTSL levels can inhibit S protein-mediated viral entrance into Calu-3 cells, a phenomenon amplified in the absence of a functional S1/S2 site.
Conclusions
The study findings demonstrated that none of the tested SARS-CoV-2 mutations at the S1/S2 sites enriched S protein cleavage, yet many diminished the cleavage of S protein at the S1/S2 sites. These mutations included P681H and S686G, the former of which was discovered in SARS-CoV-2 Alpha (B.1.1.7) and Omicron (B.1.1.529) variants of concerns (VOCs). In addition, none of the SARS-CoV-2 S protein mutations at the S1/S2 cleavage sites lowered the cell-cell fusion and ACE2 binding. On the contrary, several of these mutations elevated the host cell entry capacity of SARS-CoV-2. The S686G mutation's impact on host entry was dependent on the kind of cells. Moreover, it might be connected to the abundance of cathepsin L for the upregulation of the SARS-CoV-2 S protein.
Overall, the present study depicts that S1/S2 polymorphisms could influence the processing of SARS-CoV-2 S protein and the entry of the virus into the host.
- Arora, P. et al. (2022) "Functional analysis of polymorphisms at the S1/S2 site of SARS-CoV-2 spike protein", PLOS ONE, 17(3), p. e0265453. doi: 10.1371/journal.pone.0265453. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0265453
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: ACE2, Alanine, Amino Acid, Angiotensin, Angiotensin-Converting Enzyme 2, Assay, Cell, Cell Culture, Cell Line, Cell Membrane, Coronavirus, Coronavirus Disease COVID-19, Cytoplasm, Enzyme, Genome, Kidney, Membrane, Mutation, Omicron, Propagation, Protein, Receptor, Respiratory, SARS, SARS-CoV-2, Serine, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Stomatitis, Syndrome, Virus

Written by
Shanet Susan Alex
Shanet Susan Alex, a medical writer, based in Kerala, India, is a Doctor of Pharmacy graduate from Kerala University of Health Sciences. Her academic background is in clinical pharmacy and research, and she is passionate about medical writing. Shanet has published papers in the International Journal of Medical Science and Current Research (IJMSCR), the International Journal of Pharmacy (IJP), and the International Journal of Medical Science and Applied Research (IJMSAR). Apart from work, she enjoys listening to music and watching movies.
Source: Read Full Article
