Combining a gene-targeted drug, a cancer-bursting virus and a drug that removes the immune system’s brake pedal can tackle thyroid cancer with newfound gusto, research has found.
The triple-threat combination attacks cancer’s ability to develop resistance to a single drug by launching a multi-pronged attack, backing it into a corner with strong results in mice.
In a new study, scientists at the Institute of Cancer Research, London, looked at thyroid cancers which express a mutated gene called BRAF, which can drive cancer growth in these tumors. A game-changing drug called a BRAF inhibitor, which targets this genetic mutation, was developed at the ICR, and produces significant results in both thyroid cancers and melanomas which carry the mutation.
The cancer soon outsmarts the drug in many cases, however, with the drug losing effect over time and allowing the cancer to get the upper hand once more.
Combination treatment
In this research, published in the Journal for ImmunoTherapy of Cancer, scientists sought to combine three modes of treatment in one, targeting the genetic fault while also stimulating the immune system into action against the tumor at the same time.
The BRAF drug, called PLX4720, had its expected effects, working well against the tumors in mice in the first instance. The team then used a type of genetically engineered herpes oncolytic virus as well as antibodies called checkpoint inhibitors.
A combination of all three saw mice survive longer and the size of their tumors shrink. Compared to the control group, mice who received the combination survived for 66% longer.
Using viruses to beat cancer
A virus similar to the one used in this study, called T-VEC, is approved for clinical use. T-VEC—a viral immunotherapy—is a herpes simplex virus type 1 which has been modified to target tumor cells. So far it has only been approved for use in advanced-stage melanoma but is in clinical trials for other forms of cancer, as a single treatment or in combination with other immunotherapy treatments.
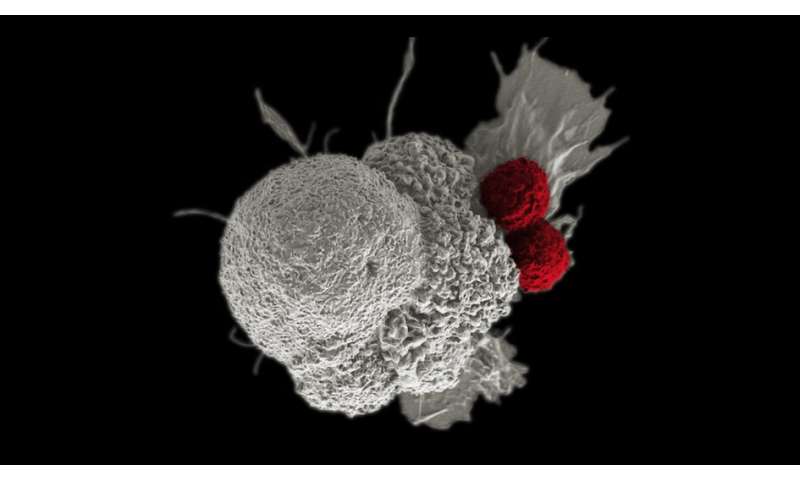
Though these types of viruses are intended to have a direct killing effect against cancer cells, what makes the oncolytic viruses even more useful is their ability to cajole the immune system into action in a localized way—raising a flare to key immune cells such as T cells that they should come and deal with the tumor.
The ICR and The Royal Marsden NHS Foundation Trust played a central role in the development of anti-cancer oncolytic herpes viruses, with Professor Kevin Harrington, Professor of Biological Cancer Therapies at the ICR, leading this pre-clinical study, and the phase I, II and III clinical trials of T-VEC.
Combatting cancer resistance
Combination treatments such as this are one way that scientists hope to help overcome cancer drug resistance, which is a major focus of work at the ICR. The ICR’s new Center for Cancer Drug Discovery is a state-of-the-art drug discovery center, which aims to create more and better drugs for cancer patients.
The Center will host the world’s first “Darwinian’ drug discovery program, designed to tackle cancer’s lethal ability to evolve resistance to treatment. Researchers aim to develop a new generation of drugs that will make the difference to the lives of millions of people with cancer.
“These are really promising results, showing three is the magic number when it comes to combining therapies for thyroid cancer” explains Professor Alan Melcher, Professor of Translational Immunology at the ICR.
“This study gives us a great basis to investigate the role of T cells further, and work out how they do their job in cancer. We hope to be able to combine these treatments in clinical trials in future to make a real difference for patients, and help nip cancer drug resistance in the bud by attacking from all angles.
Source: Read Full Article
