“Try to lose weight!” Patients with overweight seldom manage to follow their doctor’s advice. By failing to do so, there is a risk that their unwanted kilograms will weigh heavily on their kidneys, among other things.
Austrian researchers have some good news regarding this frustrating situation. It’s not the excess weight itself that is the cause of kidney failure but rather being overweight and having an unfavorable metabolic profile. Therefore, a healthier lifestyle and taking medication could lead to great improvements.
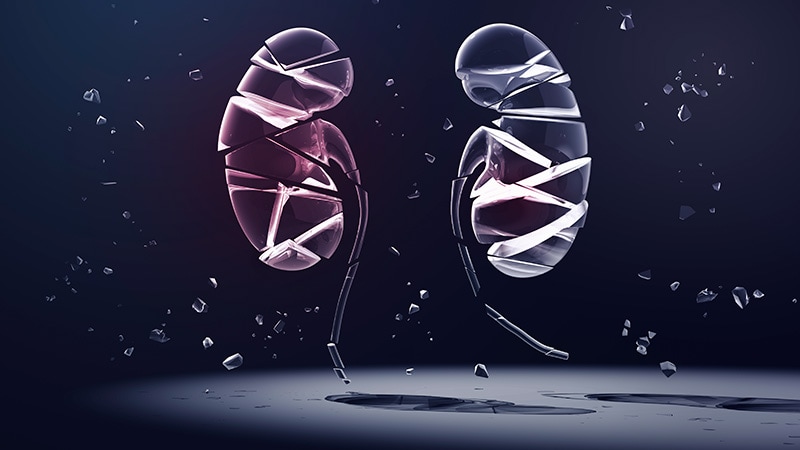
People with overweight are at greater risk for kidney failure. For example, people with a body mass index (BMI) of 30 are almost 2.5 times more at risk than those of normal weight, explained Josef Fritz, PhD, and his colleagues from the Medical University of Innsbruck in a study published in the Journal of the American Society of Nephrology.
What Damages the Kidneys?
Is it actually the extra pounds themselves, or is it the extra pounds and other concomitant (ie, indirect) factors that contribute to the final stages of kidney diseases? And to what extent?
“We expected insulin resistance and high blood pressure to represent a significant proportion, almost a third, by our calculations,” Fritz told Medscape Medical News. Surprisingly, elevations in uric acid levels accounted for a further third.
“This has barely even been considered in the specialist literature. A key message to physicians therefore would be to also pay attention to uric acid levels and to recommend to patients that they restrict anything that could increase these levels,” said Fritz. Such factors include consuming alcoholic drinks, drinks that contain fructose, and eating candy and purine-rich, foods such as meat, fish, or legumes. If these measures do not lead to a reduction in uric acid levels, medicinal products, such as allopurinol, are available.
Increased Cholesterol?
The biostatistician added, “In contrast, the effect of increased cholesterol levels, which are highly relevant for cardiovascular diseases, is very minor for end-stage kidney diseases, at 2%. There is a remainder of just 1% for excess weight as its own indirect risk factor.”
The scientists used a relatively new parameter to measure insulin resistance — the TyG index, which is the logarithmic product of triglyceride and glucose levels. They consider the TyG index, which is highly informative and easy to determine, to be a surrogate marker.
According to a previous study, insulin resistance is of special importance, since there is evidence that glucose conversion is disrupted early on in people with overweight. This disruption facilitates kidney diseases, even if diabetes is not yet present (see box).
Everything Is Intertwined
“However, it should not be inferred from this that the individual components are clearly distinct from one another in practice. In fact, they go hand in hand,” emphasized Fritz. By improving metabolic status through a balanced diet and exercise, then weight is usually reduced automatically.
If weight loss is primary, then benefits occur with regard to insulin resistance and a reduction in blood pressure and uric acid levels — as the saying goes, killing multiple birds with one stone.
The researchers used a complex mediation model for their analysis, which, unlike traditional methods, allowed the influences on a later event to be broken down into direct and indirect components.
Dialysis or Transplantation
They used this model to calculate that an unfavorable metabolic profile is associated with a 3.6 times’ higher risk of dialysis or transplantation, regardless of BMI. “This result emphasizes how crucial it is to monitor the risk factors identified to preserve kidney function,” explained Fritz.
This finding is also true for people of normal weight (BMI 20 – 25), 17% of whom still exhibited insulin resistance, high blood pressure, and hyperuricemia in the study. However, the frequency of these problems increased to 40% for people with overweight (BMI 25 – 30) and up to 60% for people with obesity (BMI >30). “The more someone weighs, the greater the probability that standard levels have been exceeded,” said Fritz.
This trend was reflected in the figures for terminal kidney failure. From a total of 100,000 person-years, the incidence rate was 13 for people of normal weight, 22 for people with overweight, and 40 for people with obesity.
Normal Weight No Panacea
This does not mean that “unhealthy” people of normal weight necessarily have better prospects than “healthy” overweight people. The risk of dialysis or transplantation is 4.5 times higher instead of only 2 times higher respectively in comparison to the ideal scenario, which is being of normal weight with no risk factors. The worst-case scenario is the combination of “obesity plus risk factors,” which entails an almost 6 times’ higher probability.
“It has long been known that a higher BMI frequently leads to kidney diseases. However, the realization that there is such a discrepancy between metabolically healthy and unhealthy profiles is new,” said Fritz.
The data for the study came from the Vorarlberg Health Monitoring and Promotion Program (VHM&PP), which began in 1985. In this program, every adult in the state of Vorarlberg in Austria is invited to be examined by a local general practitioner. The examination involves a height and weight measurement, questions regarding smoking status, and the taking of a fasting blood sample.
Every Citizen Invited
The researchers selected just over 100,000 people enrolled in the program between 1988 and 2005 (average age, 46 years). Most had no health problems initially. One third of participants had an unfavorable metabolic profile, 41% of the participants were overweight, and 14% were obese.
The researchers combined the VHM&PP data with the Austrian dialysis and transplantation register, which contains a record of every kidney replacement therapy in the country. From the pooled data, they found that 463 participants (0.5%) had required dialysis or transplantation during the average observation period of 23 years, mostly owing to a diabetic or vascular kidney disease.
Fritz noted that the size of the cohort and the length of the observation period were strengths of the study. “Through this alone, we had the opportunity to record the case numbers in the most reliable manner possible and thereby to determine the BMI-related associations with the kidneys.”
How Insulin Resistance Damages the Kidneys
Regardless of whether diabetes develops later or not, insulin resistance and poor kidney function potentiate each other in a vicious circle. This is because both insulin receptor isoforms are expressed in the kidneys, by which the hormone acts directly on the glomerular endothelium, podocytes, and tubular epithelial cells. This sets in motion signaling pathways that are important for both function and structure.
Insulin resistance upsets the balance of these processes, which leads to glomerular hyperfiltration, sodium retention, inadequate tubular reabsorption, inflammation, and fibrosis. In turn, these disruptions cause the insulin resistance worsen (source: Medicom).
This article was translated from the Medscape German edition.
Source: Read Full Article