Two new reports from researchers at the University of Tennessee Health Science Center provide the first published description of unplanned interruptions in radiation cancer treatment across a major U.S. city in the COVID-19 era, according to their authors. The studies placed special focus on how risk for radiotherapy interruption varied by patient race, socioeconomic status, and home neighborhood.
According to the researchers, the initial article, published in the International Journal of Radiation Oncology—Biology—Physics, provides the first report of how interruption rates were impacted by the COVID-19 pandemic across a U.S. metropolitan region. The second, published in Advances in Radiation Oncology, studied interruptions in cancer radiation treatment associated with unplanned hospitalization during therapy.
David Schwartz, MD, professor and chair of the Department of Radiation Oncology in the UTHSC College of Medicine, led the team that performed the work.
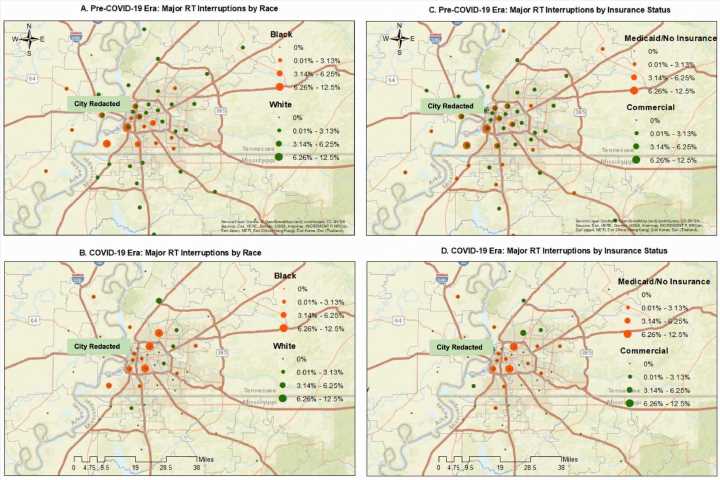
The COVID-19 manuscript documented a persistent 36% overall decline in patient volume across the first pandemic year. Although overall interruption rates trended slightly downward during the first pandemic year, financially disadvantaged populations undergoing longer planned courses of radiotherapy remained at risk for major gaps in treatment.
Detailed geospatial analysis of Memphis added critical insights, revealing interruption risk concentrating within racial minority communities living in urban downtown neighborhoods. The authors noted their findings could be leveraged to design strategies to enhance access to treatment in specific communities well beyond the pandemic.
In the second article, Dr. Schwartz’s team reviewed five years of radiation treatment records at UTHSC to catalog associations between unplanned hospitalization events and radiotherapy interruption. The three most common causes for hospitalization were malnutrition/dehydration, respiratory distress/infection, and fever/sepsis. The team identified factors predictive for interruption coinciding with hospitalization, including African American race, Medicaid/uninsured status, and having lung or throat malignancies.
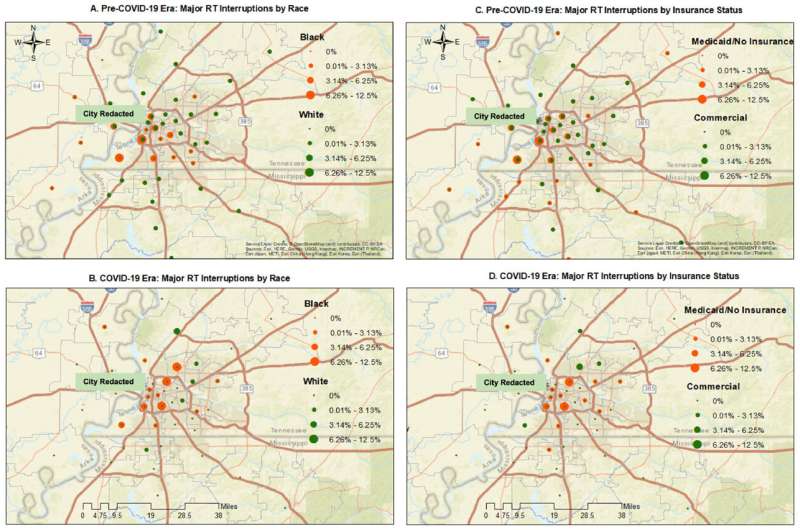
The team again leveraged geospatial mapping to find interruption events clustering among uninsured/Medicaid patients living in urban, low-income, majority African American neighborhoods. However, these events were not limited to poor neighborhoods. Patients from middle-income suburban communities were also impacted.
“Associations between hospitalization and treatment interruption were driven by location. Risk was observed in poorer urban neighborhoods and middle-income suburban locations alike, independent of patient race. Only the wealthiest residential areas enjoyed low interruption rates,” Dr. Schwartz said.
“Patients who have the greatest access to financial resources also frequently have access to interpersonal support and social resources to keep them out of the hospital during radiotherapy,” Dr. Schwartz said. “The best way to make cancer care equitable is to bring relevant resources directly to patients that don’t benefit from that level of support.”
Dr. Schwartz’s team is now actively working to make these resources available to all Memphis communities. He serves as one of the lead investigators of a multidisciplinary program at UTHSC focused on automated identification of patients at risk for treatment interruption, coupled with downstream community-based patient support tailored to individual patient needs.
More information:
Elizabeth Gaudio et al, Defining Radiation Treatment Interruption Rates During the COVID-19 Pandemic: Findings From an Academic Center in an Underserved Urban Setting, International Journal of Radiation Oncology*Biology*Physics (2022). DOI: 10.1016/j.ijrobp.2022.09.073
Adam Hubler et al, Independent Predictors for Hospitalization-Associated Radiation therapy Interruptions, Advances in Radiation Oncology (2022). DOI: 10.1016/j.adro.2022.101041
Journal information:
International Journal of Radiation Oncology*Biology*Physics
Source: Read Full Article