The European Society of Cardiology (ESC) has issued new guidelines for the prevention, diagnosis, and management of infective endocarditis (IE) — a rare and potentially lethal inf2ection of the heart’s lining and valves.
The document revises the 2015 version, based on advances in imaging and a trial of antibiotic prophylaxis, among other new developments.
Co-chairpersons of the writing task force, Victoria Delgado, MD, PhD, and Michael A. Borger, MD, PhD, and other members presented and discussed the guidelines in three packed sessions at the European Society of Cardiology (ESC) 2023 Congress, and the document was simultaneously published online in the European Heart Journal.
Endocarditis “can present with so many different clinical scenarios, so making the diagnosis can be very challenging,” Borger, from the Heart Center of Leipzig, Germany, told theheart.org | Medscape Cardiology in an interview.
Diagnosing a lethal, rare, but not uncommon disease such as endocarditis “is something that clinicians struggle with every day,” he noted, pointing to the large overflowing auditoriums where these guidelines were presented.
Borger identified four main takeaways from the document:
-
Increased level of recommendation and a clearer definition of prevention and prophylaxis of endocarditis in higher-risk patients.
-
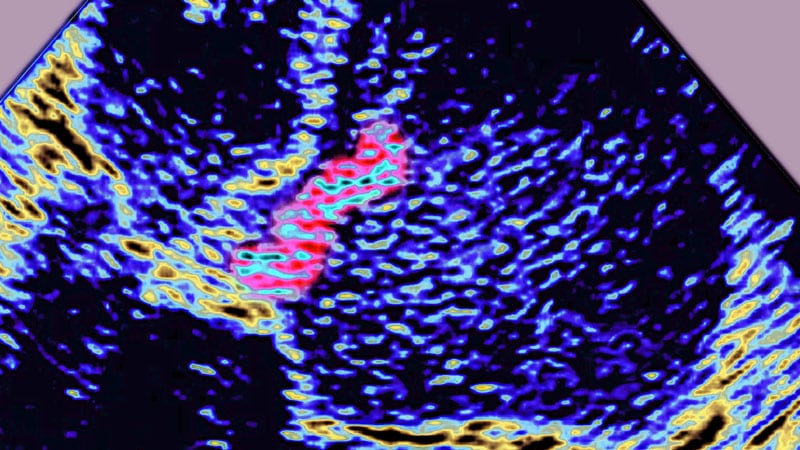
An increasing role of nonechocardiographic, advanced cardiac imaging techniques in the diagnosis of endocarditis. “The advanced cardiac imaging techniques achieved the same level of recommendation as echocardiography,” he noted.
-
More precisely defined indications for surgery and the timing for surgery, as well as a couple of new surgical recommendations.
-
More precisely defined criteria for diagnosing and managing cardiac electronic implantable device (CIED)–associated endocarditis.
The guidelines identify patients at high risk for IE as those with previous IE and patients with surgically implanted prosthetic valves, certain congenital heart diseases, surgery with prosthetic material, or a ventricular assist device as destination therapy and recommend giving them prophylactic antibiotics before oral or dental procedures.
Patients at intermediate risk for IE include those with rheumatic heart disease, nonrheumatic degenerative valve disease, congenital valve abnormalities, CIEDs, and hypertrophic cardiomyopathy. They should be evaluated on a case-by-case basis for this prophylaxis, the guideline authors write.
Making the Diagnosis
Advances in imaging techniques necessitated a revised version of the endocarditis guidelines, Borger noted.
Patients are classified as having a definite, possible, or rejected diagnosis of IE (where a definite diagnosis requires two2 major criteria, or one major criterion and at least three minor criteria, or five minor criteria).
The two major criteria are blood cultures positive for IE and imaging positive for IE by transesophageal echocardiography, transthoracic echocardiography, or — what is new — cardiac computed tomography (CT), 18F-fluorodeoxyglucose positron emission tomography, or white blood cell single photon emission tomography/CT.
The five minor criteria are predisposing conditions, fever (temperature >38 °C), embolic vascular dissemination, immunologic phenomena, and microbiological evidence.
Patient Education
Patient education is “paramount to early diagnosis and treatment,” Delgado, from Germans Trias i Pujol Hospital, Barcelona, Spain, said in a press release from the ESC. “Those with valvular heart disease or previous heart valve surgery should be particularly diligent with regards to prevention and recognizing symptoms.”
IE occurs when bacteria or fungi enter the bloodstream, for example through skin infections, dental procedures, and surgery. Symptoms include fever, night sweats, unexplained weight loss, cough, dizziness, and fainting, the press release notes.
“We have several clinical scenarios that are increasing,” Delgado said at an Ask the Experts session, including implanted cardiac electronic devices, new transcatheter therapies, and increasing endocarditis in people who use injection drugs, “and we have recommendation of evaluation of these patients at follow up.”
“The guidelines have 34 new recommendations,” she noted in a Guideline Overview session. She drew attention to a central figure, “where we tried to summarize the pathway of the patient who is diagnosed with endocarditis, and where we highlight the role of the endocarditis team,” she said.
The guidelines specify a prophylactic antibiotic regimen for high-risk dental procedures, for children and for adults with or without allergy to penicillin or ampicillin, given as a single dose 30 to 60 minutes before a procedure, she noted.
A new recommendation is that systemic antibiotic prophylaxis may be considered for high-risk patients undergoing invasive procedures of the respiratory, gastrointestinal, or genitourinary tract; skin; or musculoskeletal system.
“It is very important to have a well-educated population,” Delgado stressed.
Figure 2 of the guideline depicts what patients should do, she said, such as “maintain good dental hygiene, avoid tattoos and piercings, be mindful of infections, do not self-prescribe antibiotics.” This card can be given to the patient, and they can show it to doctors before interventions.
The main targets for antibiotic prophylaxis are oral streptococci, but the emerging and increasing resistance of these bacteria are reasons why patients should not self-prescribe, Delgado noted.
“Patients should not be self-medicating in order to try to lower their risk of endocarditis,” Borger said. “They should be speaking to their physicians and have their physician group them according to their risk category.”
“If they are low risk, there’s no reason to take antibiotic prophylaxis [before oral or dental procedures], but if they are high risk, they should not only be taking antibiotic prophylaxis, they should also be doing things like good dental hygiene — visiting the dentist once or twice a year, avoiding unnecessary procedures such as tattooing and piercings, and quick aseptic management of skin wounds.”
POET Trial: Earlier Shift to Oral Antibiotics at Home
“Another very important point is the increasing use of oral outpatient antibiotic therapy based on the Partial Oral Treatment of Endocarditis (POET) randomized trial,” Borger observed. “That’s a new recommendation,” he said, “with significant implications for the care of patients with this oftentimes life-threatening disease.”
In POET, patients in stable condition who had endocarditis on the left side of the heart caused by streptococci, Enterococcus faecalis, Staphylococcus aureus, or coagulase-negative staphylococci were randomly assigned to continue treatment with intravenous (IV) antibiotics (199 patients) or to shift to step-down treatment with oral antibiotics (201 patients) after at least 10 days of initial treatment with IV antibiotics.
The 5-year results were published in 2019 in the New England Journal of Medicine and presented at ESC that year. “We were hoping or expecting to see that oral outpatient therapy would be equivalent to inpatient IV therapy,” Borger said, “but we were surprised to see that oral outpatient therapy was actually statistically significantly better in terms of survival, a very hard outcome, at 5 years after the randomization.”
“This was an important part of our new guideline document. In select in patients who are ‘clinically stable’,” as defined in the guidelines, he said, “they could be successfully managed at home with oral antibiotics, rather than keeping them in hospital the whole 6 weeks.”
“In the US and in Canada, a lot of patients are sent home for intravenous therapy, whereas that practice doesn’t exist in a lot of places in Europe. The patients are sitting in the hospital here for 6 weeks, oftentimes for no other reason just to get their IV antibiotic therapy. The POET trial has shown us that that is probably the wrong thing to be doing.”
Earlier Surgical Intervention
The new guidelines also recommend that “once there is an indication to do cardiac surgery, it should be promptly performed,” Borger noted.
Surgery to remove infected material and drain abscesses is indicated for patients with heart failure or uncontrolled infection and to prevent embolism.
“We have defined emergency indications that should be done within 24 hours; urgent, which should be done within 3 to 5 days; and nonurgent, more than 5 days but within the same hospitalization,” he elaborated. “We’re basically trying to encourage surgeons and nonsurgeons that once there is an indication for surgery, there’s not a lot of benefit to just waiting. You should proceed with operation in a timely manner” to improve survival.
The guidelines recommend surgery for early prosthetic valve endocarditis, within 6 months of valve surgery, with new valve replacement and complete debridement.
Patients who present with stroke and require surgery are not uncommon, Borger noted. Ischemic stroke should not be a reason to delay surgery, and patients with hemorrhagic stoke, with favorable features, can undergo surgery.
The guidelines provide a figure for the management of CIED-related infective endocarditis. They also include a new section devoted to patient-centered care and shared decision making.
The guidelines were endorsed by the European Association for Cardio-Thoracic Surgery (EACTS) and the European Association of Nuclear Medicine (EANM). The writing task force included representatives from EACTS, EANM, and the European Society of Clinical Microbiology and Infectious Diseases.
The complete guidelines, as well as pocket guidelines, essential messages, a pocket guidelines app, and an official guidelines slide set, all addressing endocarditis, are available from the ESC website.
The guidelines did not receive any funding. The disclosure forms of all experts involved in their development are available on the ESC website .
European Society of Cardiology (ESC) 2023 Congress. Presented August 25, 2023.
Eur Heart J. Published online August 25, 2023. Full text
For more from theheart.org | Medscape Cardiology, join us on Facebook, X (formerly known as Twitter), Instagram, and YouTube
Source: Read Full Article