A study by Queen Mary University of London researchers, funded by Cancer Research UK, confirms the role of the oestrogen receptor biomarker in ductal carcinoma in situ and presents a new and more accurate method to predict long term outcomes for this pre-invasive stage of breast cancer. The study is published in Clinical Cancer Research.
Oestrogen receptor (ER), a protein expressed in some breast cancer cells, is routinely tested in invasive breast cancer to predict long-term outcomes select treatment options. Its role in ductal carcinoma in situ (DCIS) has been previously unclear, and it is not generally evaluated in this pre-invasive stage of breast cancer. The new research confirms the role of ER in predicting long-term outcomes in DCIS, and the authors report a new and more accurate method to evaluate ER for predicting long-term outcomes in DCIS.
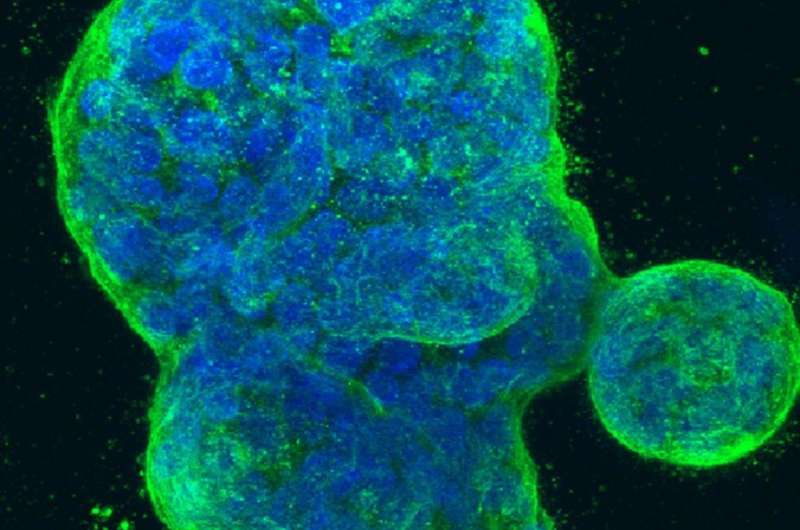
This is the first study to use samples from a randomised trial (the UK/ANZ DCIS trial) to investigate ER as a prognostic marker in DCIS. The researchers observed multi-clonality in ER expression in 11% of ER-positive DCIS (ie: ER-positive DCIS with distinct ER-negative clones) and investigated the prognostic role of such multi-clonality in ER expression. They found that ER is a strong prognostic factor with greater than 3-fold risk of ipsilateral recurrence in ER-negative DCIS, and therefore conclude that ER should be routinely assessed in DCIS and that the clonal method they report should be considered.
Lead author Mangesh Thorat from Queen Mary University of London said: “It is unlikely that such a study could currently be reproduced elsewhere in the world, and the robustness of these results means we can rely on them to make changes to clinical practice. Routine testing of ER in DCIS will help to avoid both overtreatment and undertreatment in this type of breast cancer. The insights from this study will also help improve future breast cancer research through use of new scientific models, particularly in areas of drug resistance and the use of targeted therapies.”
Source: Read Full Article
