How do mutations benefit severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)? To explore this, a team of researchers from China took a closer look at the physical interactions that occur between the proteins after viral mutation.
Using molecular simulation studies, the researchers investigated the binding between the viral spike protein – where significant mutations have occurred – and its human receptor, angiotensin-converting enzyme 2 (hACE2).
They found that the mutation, E484K, drives the protein to have more favorable electrostatic interactions, thus altering its binding affinity. In short, this strengthens the bonding between the viral protein and its receptor. As an additional benefit to the virus, this mutation reduces the immune response in the host. The team has released their findings on the bioRxiv* preprint server.
.jpg)
SARS-CoV-2 is the etiological agent of the current pandemic coronavirus disease 2019 (COVID-19). It was first identified in December 2019, in Wuhan, China. Since then, the virus has infected more than 109 million people worldwide and caused over 2.4 million deaths.
However, some newly emerged variants are highly transmissible and infectious. It is important to investigate the molecular mechanisms of these naturally occurring mutations, their impact on the infectivity of the SARS-CoV-2, and the subsequent efficacy of the current vaccines in promoting immunity.
The SARS-CoV-2 is a highly transmissible and pathogenic coronavirus. The viral genome is single-stranded RNA which is enveloped by a lipid membrane embedded with proteins. The protruding spike (S) protein present on the virus's surface binds to the receptor hACE2 on the host cell to enable its entry. The S protein is a homo-trimeric glycoprotein, with each protomer composed of S1 and S2 subunits.
Conformational transitions of the receptor-binding domain (RBD) on the S1 subunit cause the virus to recognize and bind with the hACE2. This binding then triggers membrane fusion and infiltration of the virus into the host cell, wherein it hijacks the cell’s metabolic mechanism to commence viral replication. Thus, the RBD predominantly determines the infectivity of the SARS-CoV-2. The RBD region contains the major neutralizing epitopes and is the target of antibodies.
The fast-evolving SARS-CoV-2 has emerged into several variants: namely, B.1.1.7 or 501Y.V1; B.1.351 or 501Y.V2; P.1 or 501Y.V3. Most of the mutations reside in the receptor-binding motif (RBM) of the RBD on the S protein. Early studies of these variants suggest heightened transmissibility compared to the original SARS-CoV-2 strain.
Of these mutations – N501Y, E484K and K417N (or K417T) – the E484K mutation (which is shared by both the 501Y.V2 and 501Y.V3 variants), is named the “escape mutation” because it distinctly reduces the neutralization activity of and may also escape from the neutralizing antibodies in the convalescent plasma of COVID-19 patients. This may also weaken the effectiveness of the currently approved vaccines and the efficacy of the neutralizing antibody therapeutics currently in development.
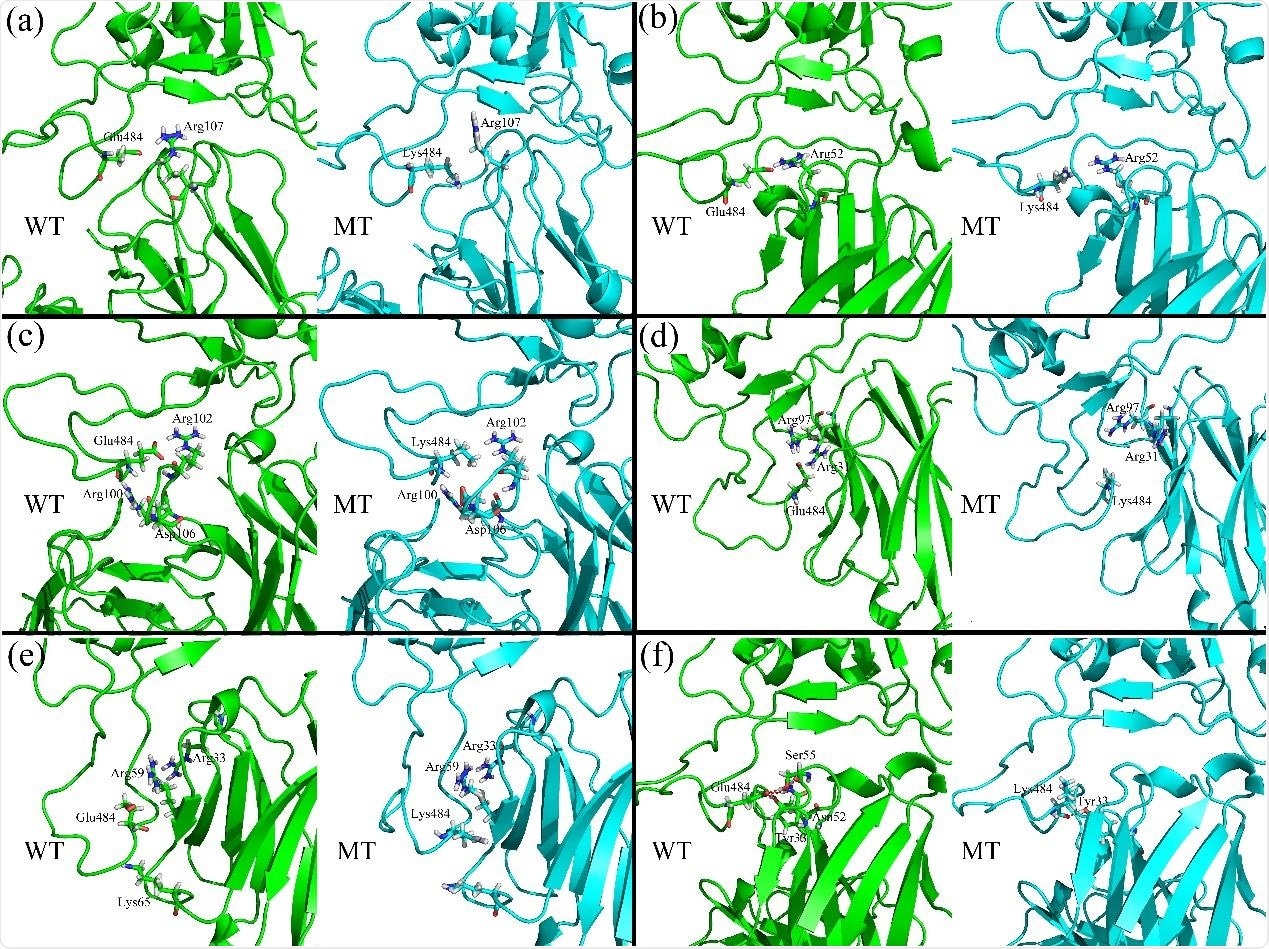
Amid this mounting concern, the researchers probed the impacts of E484K mutation on the virus’s binding affinity. They further investigated the impacts of E484K mutation on the binding affinities of RBD with the neutralizing antibodies and nanobodies.
They investigated these molecular mechanisms using the molecular dynamics (MD) simulations combined with the molecular mechanics-generalized Born surface area (MMGBSA) method. They evaluated the receptor binding free energy both for the wild-type RBD and the E484K mutant.
They found that the E484K mutation may improve the binding affinity of RBD to the receptor hACE2. This occurs because of more favorable electrostatic forces and a tighter binding interface caused by the mutation. Conformational rearrangements of the local structure around the mutant residue and the formation of more hydrogen bonding added to the bond's strength.
This implies that the E484K-containing variant is endowed with boosted transmissibility. Also, for most of the studied neutralizing antibodies and nanobodies, the researchers found that the E484K mutation reduced the binding affinities between RBD and these antibodies.
This is mainly observed due to the mutation-caused disadvantaged electrostatic interactions, which weakened the effectiveness of these antibodies, the researchers explain.
This study revealed that the E484K mutation might improve the binding affinity between the RBD and the receptor hACE2 – implying more transmissibility of the E484K-containing variants. This is evident from the current data from the variant-infected regions. And the mutation also weakens the binding affinities between RBD and the studied neutralizing antibodies, indicating reduced effectiveness of these antibodies. This is alarming in the face of vaccine roll-out currently happening across the world.
This study discovers the benefits the virus derives from the mutation. The results provide valuable information for the effective vaccine development and antibody drugs design, the researchers write.
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Wei Bu Wang, Yu Liang, Yu Qin Jin, Jing Zhang, Ji Guo Su, Qi Ming Li. (2021) E484K mutation in SARS-CoV-2 RBD enhances binding affinity with hACE2 but reduces interactions with neutralizing antibodies and nanobodies: Binding free energy calculation studies. bioRxiv 2021.02.17.431566; doi: https://doi.org/10.1101/2021.02.17.431566, https://www.biorxiv.org/content/10.1101/2021.02.17.431566v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News | Healthcare News
Tags: Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Antibody, binding affinity, Cell, Convalescent Plasma, Coronavirus, Coronavirus Disease COVID-19, Drugs, Efficacy, Enzyme, Genome, Glycoprotein, Immune Response, Mutation, Nanobodies, Pandemic, Protein, Receptor, Respiratory, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Therapeutics, Vaccine, Virus

Written by
Dr. Ramya Dwivedi
Ramya has a Ph.D. in Biotechnology from the National Chemical Laboratories (CSIR-NCL), in Pune. Her work consisted of functionalizing nanoparticles with different molecules of biological interest, studying the reaction system and establishing useful applications.
Source: Read Full Article
