- During a nuclear bone scan, known as bone scintigraphy, patients may unexpectedly show high levels of DPD uptake (a cardiac radiotracer), indicating the presence of cardiac amyloidosis.
- Previously thought to be uncommon, recent advancements in diagnosis have revealed higher rates of CA than previously known.
- Now, new research has found that about 3% of individuals who undergo bone scans exhibit signs of CA, helping to gain further information on the occurrence and effects of this condition among the general population.
Cardiac amyloidosis (CA) causes the heart to thicken and become inflexible due to abnormal deposits of protein in place of healthy heart tissue.
The best way to treat this disease is to catch it early before it progresses. Otherwise, it can result in heart failure and even death.
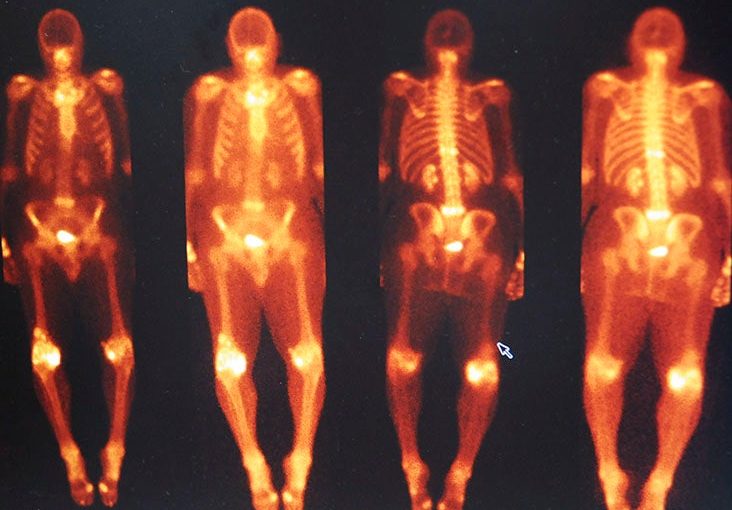
A DPD scan is an imaging test that helps doctors diagnose CA. It uses a small amount of a radioactive substance called technetium-99m (99mTc) and a chemical called DPD.
During the test, these substances are injected into the body and then a special camera takes pictures of the heart. These images can show if the heart has abnormal deposits of the amyloid protein.
Amyloid deposits cause the heart muscles to become rigid, which makes it harder for the heart to pump blood throughout the body. Bone scintigraphy is therefore used to help doctors see how much amyloid has built up and how it is affecting the heart.
Since cardiac amyloidosis can lead to serious outcomes, it is crucial to accurately diagnose DPD uptake by the heart. People who display DPD uptake should be directed to a cardiologist for additional evaluation.
A new study, published in The Journal of Nuclear Medicine, is designed to determine the occurrence of cardiac amyloidosis in the general population through bone scans and to examine its impact on people with the condition.
What did the study involve?
Researchers recruited 11,527 individuals who received either cardiac or non-cardiac referrals and underwent DPD bone scintigraphy, generating a total of 17,387 scans.
Nuclear medicine experts examined all the scans, and based on visual analysis, they categorized the scans as grade-0 (no DPD uptake), grade-1 (some DPD uptake), and grade-2/3 (indicating the presence of cardiac amyloidosis).
Out of all the subjects who participated in the study, slightly more than 3% showed some degree of DPD uptake, with nearly 2% classified as grade-1 and slightly more than 1% as grade-2/3.
The prevalence of DPD uptake was estimated to be 1 in 50 for non-cardiac referrals and 1 in 5 for cardiac referrals.
The prevalence of DPD uptake increased significantly with age and those with DPD uptake were more likely to have age-related conditions such as high blood pressure, coronary artery disease, and impaired kidney function.
Following an average of six years of monitoring, almost 30% of the subjects died and cardiovascular-related fatalities made up nearly 9% of those deaths.
During the follow-up period, slightly more than 1% percent of participants had to be hospitalized for heart failure. Patients with grade-2/3 DPD uptake were found to be 3 times more likely to be hospitalized for heart failure than those with grade-0 uptake.
Experts react to the cardiac research
Dr. Christian Nitsche, a doctor-in-training in the division of cardiology at the Medical University of Vienna and the first author of the study, explained the background to Medical News Today.
“Cardiac amyloidosis (CA) is an infiltrative cardiac disease. Particularly Transthyretin (ATTR)-CA [which] can be diagnosed non-invasively with DPD bone scintigraphy. However, the prevalence of CA in the “general population” and associated prognostic implications are poorly understood,” Nitsche said.
Dr. Tharusha Gunawardena, a cardiologist at Ipswich Hospital in the United Kingdom who was not involved in the study, agreed.
“Cardiac amyloidosis is a challenging rare condition with an incidence of about 1 in 1,000 people with about 500 to 600 new cases in the [United Kingdom] every year (according to the UCL National Amyloidosis Centre),” Gunawardena told Medical News Today.
Diagnosis is often late and can be protracted relying on certain features on Echocardiography and Cardiac MRI. The paper is interesting in that it aims to screen for prevalence though its inherent potential for clinical application seems unclear. Some people [may have had] bone scintigraphy for cancer, but it may have been helpful to understand the non-cancer reasons for doing them.
Dr. Tharusha Gunawardena
Gunawardena noted that “patients who had bone scans had been assessed retrospectively looking at their outcomes. The isotope uptake detected for these scans was greater for patients with cardiac amyloid and the proportion of this appeared to relate to morbidity and mortality outcomes (as in the risk of adverse events and death).”
Nitsche pointed out that there were limitations to the research, saying “not all patients with DPD positivity had additional SPECT/CT imaging of the heart. Cardiac uptake of any intensity on planar imaging should always be confirmed by SPECT/CT to differentiate myocardial from other sources of tracer uptake (e.g. blood pool, ribs). This highlights the necessity of thorough assessment in case of suspected cardiac uptake.”
The research, however, has implications for patients and the public.
Patients undergoing bone scintigraphy for different reasons may present with DPD+ as an incidental finding. Facing worse outcomes and given the availability of novel treatment options for both common subtypes of CA (ATTR and light-chain CA), efforts would be maximized to reliably diagnose DPD+. Patients with DPD+ should then be referred to a cardiology specialist for further assessment and treatment initiation.
Dr. Christian Nitsche
Gunawardena agreed, saying, “[this study] would suggest that perhaps there is scope for prospective studies to explore the potential role and benefit of using bone scintigraphy in the initial assessment of patients with cardiac diagnosis.”
This may inform on [those] patients who could benefit from referral to specialist centres and perhaps more aggressive initial treatments. The effect on prognosis may help facilitate conversations with patients and families on future expected outcomes.
Dr. Tharusha Gunawardena
Source: Read Full Article