“We need a spray bottle, to spray her like a bad cat,” one of the emergency department workers said as Tolulope Afolabi protested that she was too woozy from pain medication to be hustled out of the hospital.
Afolabi, a 29-year-old Philadelphia nursing student, had come to Roxborough Memorial Hospital hours earlier that night by ambulance, delirious with a body-breaking pain that she described as like an SUV rolling over her back. She was met by emergency room staff who, after treating her with IV pain medication, tried to discharge her before she was even able to walk straight.
By the time of this March 2019 encounter, Afolabi had had so many similar encounters in hospitals that she discreetly captured it on an Instagram livestream, so friends would know how to find her if she needed help and so no one could say it hadn’t happened. She shared it with The Inquirer.
In the recording, staff can be heard ordering Afolabi to sit down in a chair—”What is so hard about you sitting in a chair?” one chides—and laughing when she struggles to explain she is nauseated and in pain.
“There is a lot going on when I move that brings up the pain,” she says, her voice raw from screaming in agony earlier that evening, each word enunciated carefully to cut through the medication fog.
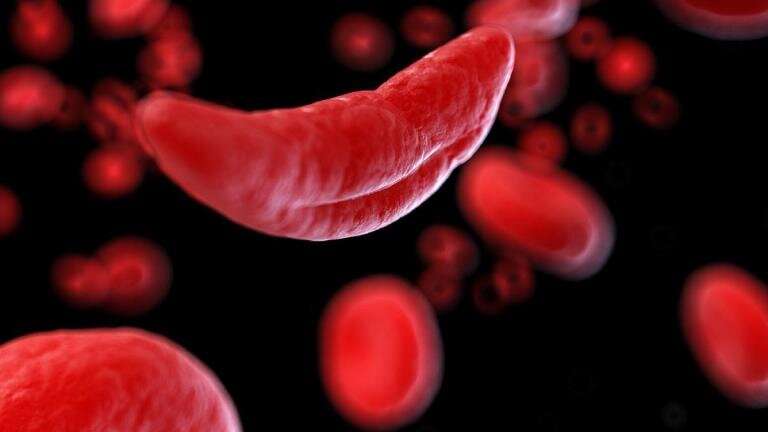
Afolabi was born with sickle cell disease, a blood disorder which affects every organ of the body and leads to unpredictable pain crises. Despite some 100,000 people in the U.S. living with sickle cell disease, the condition—which is most common in but not exclusive to people of sub-Saharan African ancestry—is under-resourced and misunderstood.
“I’ve been called dramatic. If you felt half of what I’ve felt, you’d never call me dramatic,” Afolabi said. “I can’t do anything but cry and scream because I have no release for the pain.”
Until infant screening for the disease became routine in the 1980s, few people born with the disorder lived past childhood. With early diagnosis and treatment, patients are increasingly living into adulthood, but when they age out of the pediatric system, they encounter a system that can be so harsh and unsupportive, some do all they can to avoid seeking care until their pain is unbearable.
They struggle to book appointments with the few sickle cell specialists for adults, and are often accused of seeking opioids when they get emergency care.
Sickle cell patients and advocates say their suffering is largely the result of the systemic racism in society generally and health care specifically that the coronavirus pandemic has cast in sharp relief. And with a social justice movement sparked by George Floyd’s murder gaining momentum, advocates say now is the time to fix the system.
“This journey is not unique to the sickle cell population,” said Kim Smith-Whitley, director of the Comprehensive Sickle Cell Center at Children’s Hospital of Philadelphia. “Given the sociopolitical environment in the U.S., I think we know this is a population that has not gotten what they need. This is our opportune time to correct it.”
First recognized in the U.S. in the early 1900s, sickle cell disease was among the first group of conditions understood to be the result of a genetic mutation, a discovery that contributed to the foundation of genetic and molecular biology.
About 1 out of every 365 Black babies are born with sickle cell disease, which occurs when round red blood cells take on the C-shape of a farming sickle and grow hard and sticky, making them unable to carry adequate oxygen to vital organs. Another 1 in 13 carry the sickle cell trait. The disease—actually a group of four diseases that include sickle cell anemia—can only occur when both parents carry the trait.
Episodes of extreme pain, called a sickle cell crisis, require hospital treatment and are the hallmark of the disease. But many people with the disease are in constant pain or discomfort. Young adults often need joint replacements to repair bone deteriorated by the disease.
Internal organ destruction can be so swift that, decades ago, few patients lived to adulthood. Children began living longer when, in the 1970s, a national awareness campaign prompted the federal government to spend more on research and care. One resulting study found that penicillin taken twice daily could protect children from overwhelming infection, prompting widespread newborn screening in the late 1980s.
With early diagnosis, blood transfusions and close management have helped the vast majority of individuals with the disease live to adulthood. People born today with sickle cell disease can expect to live into their 50s, up from their mid-30s just a couple decades ago.
CHOP’s sickle cell program, the largest pediatric program in the Philadelphia area, has grown from about 325 patients in the early 1990s, before universal newborn screening, to over 1,000 patients. The sickle cell program’s hematologists work with primary care providers, social workers and specialists in eye, lung and heart care—organs most commonly affected by the disease.
When a child arrives in CHOP’s emergency department in crisis, staff know to alert the sickle cell team.
St. Christopher’s Hospital for Children also has a robust, though smaller, sickle cell program. Most pediatric sickle cell patients in the Philadelphia area are treated by one of the two programs, Smith-Whitley said.
The key to their success, Smith-Whitley said, is recognizing that “sickle cell doesn’t just occur in the context of a hospital visit, but in a life.”
But after childhood, sickle cell patients feel like they’re stepping into a health care void.
Or, as the director of Penn Medicine’s sickle cell program, Farzana Sayani, puts it, “And then everything falls apart when they become adults.”
Young adults may begin to experience different symptoms as they mature. They may be learning how to manage their health, without help from parents. At the same time, they are transitioning into an adult health care system that lacks wraparound services such as social workers and nurses who check in periodically, just to see how they’re doing.
Shanika Walls, 26, of Philadelphia, was diagnosed with sickle cell disease when she was 3, and stayed with her CHOP care team as long as she could. One doctor came home from vacation early to be with her when she needed emergency surgery to remove her appendix—a simple childhood event made traumatic by sickle cell.
Her inevitable move to an adult care team was like a baby bird being shoved from its nest into a hailstorm.
Even her first appointment felt rushed and impersonal. The doctor took her vitals and wrote a prescription for a medication Walls told the doctor was not part of her maintenance routine.
She remembers someone telling her, “This isn’t Children’s Hospital. This is an adult hospital.”
“It was very shocking to me,” she said. “From there I’ve just tried to do what I have to do at home, rather than going in.”
Her doctor wants to see her every six months, but Walls usually cancels the appointments because she does not feel that the doctors are listening to her. She takes ibuprofen and drinks lots of water to control inflammation, but worries about what will happen when she has a pain crisis and doesn’t have a doctor she trusts.
After months of searching, Terri Booker, 37, found a hematologist she likes, and has a good care plan. But even so, she has constant pain in her legs, like they’re being squeezed by someone with an unrelenting grip. When the sensation climbs up her arms and her body starts to feel heavy, she knows a pain crisis is coming.
Booker, a Philadelphia lawyer, waits until she can bear it no longer to go to the emergency department. Too often providers don’t believe her, don’t listen, and don’t know the right way to help, she said.
Research shows that Black people are more likely to report feeling ignored or not believed when they talk to doctors. Other studies have shown Black patients receive less pain medication at hospitals, largely rooted in the false belief—which until recently was actually taught in some American medical schools—that they feel less pain than white people.
“It’s the physical, but also the mental anguish of knowing people don’t want to treat you, they don’t care what happens to you. The mental toll it takes on your mind and body is devastating,” Booker said. “Stress for a sickle cell patient is another trigger. If you’re constantly stressed out, you can’t get better and then it makes you sicker.”
Booker has more mild symptoms than other people she knows, she said, but the disease has taken a personal and professional toll.
One small study among sickle cell patients in Virginia estimated that only a third of people with sickle cell disease are employed, and those with jobs miss an average of seven weeks of work due to pain.
Days after passing the Pennsylvania bar exam in 2012, Booker had a pain crisis that landed her in the hospital for a month and required another six months of recovery. She felt compelled to explain to prospective employers why her job search had been delayed and worried that divulging her medical condition might bias firms against her.
Earlier this year, Booker was laid off from her job when she was in the hospital for five days during a pain crisis. Even worse, she also lost her employer-sponsored health insurance.
“The first thing I did, I didn’t try to collect unemployment, I didn’t look for a new job, I applied for Medicaid,” she said. “Not having health insurance as a sickle cell patient is unimaginable. It’s not an option.”
Sayani joined Penn in 2013 to build up a comprehensive program for adult sickle cell patients. The program added 40 patients last year, about half of whom transitioned from pediatric care. The other half were adults in the community who were not regularly seeing a doctor, which she said speaks to the demand for more support.
One important change Sayani pushed for was an ER protocol, so that the sickle cell team is alerted when one of their patients comes to the emergency department. The approach has helped, but only works when a Penn sickle cell patient goes to a Penn hospital. The new protocol have raised awareness about sickle cell in the health system’s emergency departments, but patients may still encounter skepticism if they go to a hospital that doesn’t know them.
In 2018, Penn opened an infusion center, where people with chronic sickle cell pain episodes can come for help before the pain gets so bad they have to be admitted to the hospital for IV pain medication.
“It’s a safe space,” said Booker, who turns to the clinic when the pain becomes more than she can manage at home. “I feel comfortable going there. I don’t have to explain anything, they know.”
Infusion centers have been shown to reduce the number of ER admissions for people with sickle cell disease and the patients who use Penn’s center like it, Sayani said. But it has attracted only about 250 regular patients. Specialists estimate there are about 3,000 adults living with sickle cell disease in the Philadelphia area.
Transportation, child care and work obligations may be barriers for some to use the infusion center, which is open only on weekdays. Plus, it can take hours to complete an infusion.
Sayani said a lack of trust in doctors is also keeping people away.
“There is a lot of PTSD, there is a lot of trauma these patients face every time they go to the emergency department because of some negative experience,” she said. “The people who have bad disease and who have been in emergency departments and even in ICUs and close to death—they’re the individuals who have the hardest time trusting and sometimes that hinders their care.”
Patients who feel their doctors understand them and treat them with respect are far more likely than those who feel disregarded to follow through on medical orders, take the drugs they need and seek follow-up care when they need it, said Mary Catherine Beach, a professor of medicine at Johns Hopkins’ Berman Institute of Bioethics.
“That’s true in health care and that’s just true with authority,” she said. “If you’ve been treated badly in schools and by the police and in stores, why wouldn’t you think you were going to be treated badly by someone in the health system? You carry that forward.”
Improving sickle cell programs could be a starting place for health systems to make measurable change in addressing health disparities and racism, said Alexandra Power-Hays, a pediatrician in Chicago who specializes in sickle cell disease and has written about health disparities.
“It’s really hard to ‘study’ racial disparities because a lot of the things are nebulous, but because sickle cell disease is a diagnosis there are objective measures,” such as how long patients wait for pain medication, she said. “It can be a good starting point to help shine that light overall on racism in medicine.”
Patients say that any change should start with doctors listening more closely to them.
In Afolabi’s 14-minute recording, emergency room staff repeatedly tell her she can sit down and accuse her of insubordination. When they realize she is live-streaming the encounter, they accuse her of “doing this for attention.”
She pushes back when they try to help her to the chair again, yelling, “Time out! No!”
Someone laughs.
“You’re smiling while you’re being aggressive,” she croaks.
“Because you’re funny,” a man responds. “This is hilarious and you know it.”
They threaten to discharge her, calling out to whomever is watching her livestream to come to the hospital.
Finally, exhausted and falling asleep on her feet, ER workers ease Afolabi into a wheelchair. They wheel her into another room and leave her there, snoring, while Dateline airs in the background.
Back at home, Afolabi reported her mistreatment to hospital administrators. She received an apology letter shortly after the incident and earlier this year was invited to meet with the hospital’s leadership and board of directors.
“The pain is excruciating. I wouldn’t wish it on my worst enemy,” she recalled telling them. “But sometimes I do wish people in the medical field could experience it, just to know what it’s really like.”
In a statement, a spokesperson for Roxborough Hospital said Afolabi’s remarks had helped administrators better understand sickle cell disease.
“Everyone experiences pain differently, requiring an individualized approach to treatment,” Michelle Aliprantis said in an email. “Hearing from patients like Ms. Afolabi help hospitals like ours remove any barriers that could negatively impact the patient experience.”
Speaking to a couple dozen executives, most of whom were white, Afolabi said, was empowering but also felt like not enough.
As she read stories about the disproportionate toll the COVID-19 pandemic has had on Black individuals, and watched news footage of protests following the killing of George Floyd, Afolabi was inspired to speak out about her own experience—one she knows will resonate with so many other people who’ve been mistreated.
This fall, she will have heart surgery to stabilize an artery—a major procedure to correct an issue that, while not directly caused by sickle cell disease, is complicated by it. Recovery will be harder and longer than it is for patients without the blood condition, and the procedure’s timing could be derailed by a pain crisis, which she has at least once a month.
Still, Afolabi is determined to make her pain meaningful. She expects to finish her bachelor’s degree in nursing by the end of the year and wants to specialize in hematology. Her dream is to open a clinic for people with sickle cell disease, where she’ll take away patients’ pain and fear with battle-worn compassion.
——
What is sickle cell disease?
Sickle cell disease is a group of inherited blood disorders in which red blood cells become stiff and crescent shaped, which prevents them from delivering enough oxygen to the body. Sickle cell anemia is the most severe form of the disease, while other people have milder symptoms.
How do people get sickle cell disease and how is it diagnosed?
Sickle cell disease is inherited, which means both parents must have the disease or be carriers of the sickle cell trait. All babies are screened for sickle cell when they’re born through a routine blood test.
What is a sickle cell crisis?
A sickle cell crisis is when abnormally shaped red blood cells block blood vessels, preventing blood and oxygen from flowing properly. People with sickle cell disease commonly report a constant low-level pain, but a crisis is when the pain becomes extreme. It may affect a particular part of the body, such as a leg or arm, or full-body pain. Pain feels different for everyone. Some people describe sharp, stabbing pain, while others experience intense pressure, as if there is something heavy on their chest. Frequency and duration of crises vary—some people experience a crisis weekly while others go years without a major episode. Each crisis can last hours or even days.
How is sickle cell disease treated?
Eating healthy, drinking lots of water, exercising and limiting stress can reduce the likelihood of a pain crisis. To help cope with pain—which can be unpredictable and occur even with a healthy lifestyle—patients can take over-the-counter pain medication, use a heating pad and rest. For some, blood transfusions can help avoid pain crises. Hydroxyurea is a chemotherapy drug approved for use among sickle cell patients. Taken orally daily, it can help keep red blood cells round. Pain that becomes too intense to manage at home is treated with IV pain medication at an infusion clinic or hospital. Clinical trials are testing the possibility of using gene therapy to reverse the disease.
What resources are available for people with sickle cell disease?
The Sickle Cell Disease Association of America’s Philadelphia/Delaware Valley chapter (www.sicklecelldisorder.com) helps people living with the disease navigate the health care system, find the right doctors and connect with other patients. The group advocates for patients and helps individuals learn how to advocate for themselves. Being a self-advocate is especially important for people with sickle cell disease because they often encounter discrimination and a lack of understanding of their illness.
“The power of being a self-advocate is so important,” said Zemoria Brandon, a social worker with the local chapter.
Source: Read Full Article
