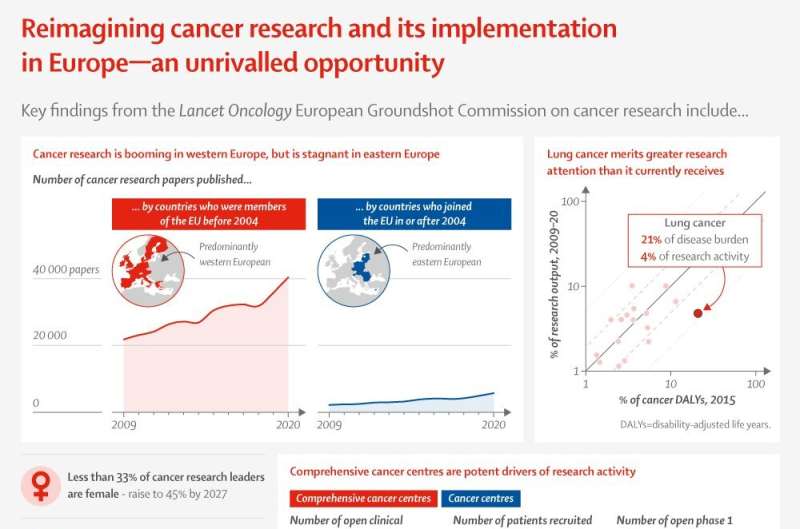
The COVID-19 pandemic has exposed weaknesses in cancer health systems and in the cancer research landscape across Europe, which, if not addressed as a matter of urgency, will set back cancer outcomes by almost a decade. In a new report, authors emphasize that prioritizing cancer research is crucial for European countries to deliver more affordable, higher-quality, and more equitable cancer care, with patients treated in research-active hospitals having better outcomes than those who are not.
The new report, European Groundshot—addressing Europe’s cancer research challenges: a Lancet Oncology Commission, brings together a wide range of patient, scientific, and health-care experts with detailed knowledge of cancer research activity across Europe. Using accurate, timely, and granular data, the report shines a penetrating light on cancer research in Europe, highlighting current and future challenges and identifying gaps within the research landscape.
The Lancet Oncology Commission echoes the US Cancer Moonshot in setting out ambitious recommendations to develop a successful and resilient cancer research roadmap. However, the Lancet Oncology Commission argues that Europe cancer research should have a more grounded, patient-focused—rather than techno-centric—approach, and therefore a “Cancer Groundshot” is a more appropriate aim.
“With the backdrop of the COVID-19 pandemic, Brexit, and the Russian invasion of Ukraine, it is more important than ever that Europe develops a resilient cancer research landscape to play a transformative role in improving prevention, diagnosis, treatment, and quality-of-life for current and future patients and those living beyond cancer,” says Professor Mark Lawler, Queen’s University Belfast, UK and Chair and lead author of the Commission.
He continues, “We estimate that approximately one million cancer diagnoses were missed across Europe during the COVID-19 pandemic. We are in a race against time to find those missing cancers. Additionally, we saw a chilling effect on cancer research with laboratories shut down and clinical trials delayed or canceled in the first pandemic wave. We are concerned that Europe is heading towards a cancer epidemic in the next decade if cancer health systems and cancer research are not urgently prioritized. Our European Groundshot Commission provides crucial findings on the current landscape of cancer research, exposes the key gaps, and demands the prioritization of European cancer research agendas over the next decade.”
European cancer research faces a triple threat
The European Groundshot Commission analyzed data on the impact of the COVID-19 pandemic across Europe and found that clinicians saw 1.5 million fewer patients with cancer in the first year of the pandemic, with one in two patients with cancer not receiving surgery or chemotherapy in a timely manner. Additionally, 100 million cancer screening tests were missed, and it is estimated that up to one million European citizens might have an undiagnosed cancer due to the cancer backlog.
Considering these findings, one of the European Groundshot Commission’s key recommendations is for the European cancer research community to accelerate the research response to the indirect impacts of the COVID-19 pandemic on cancer, and that now more than ever, there is a crucial need to ensure that cancer is appropriately protected and prioritized within current and future European research agendas.
The Russia invasion of Ukraine represents another huge challenge to cancer research in Europe. Russia and Ukraine are two of the largest contributors to clinical cancer research in the world, especially industry-sponsored clinical research. Many Ukrainian cancer clinical trials include cancer centers in central and eastern European countries, and the conflict will likely result in many of these major trials being delayed or failing to recruit.
An additional danger is that industry might consider it too high risk to run cancer clinical research in countries bordering Ukraine—loss of private sector investment would be hugely damaging to cancer research in central and eastern Europe. The European Groundshot Commission recommends that as a matter of extreme urgency, the European cancer community must gather data on the impact of the conflict on patients, cancer services, medicines and other shortages, and workforce gaps, in Ukraine and in neighboring countries, as well as developing a plan to mitigate the impact of the war on cancer research.
“Whilst there has been a lot of news coverage on the Russian invasion of Ukraine, what has gone relatively unreported is its profound and continuing impact on clinical cancer research. We hope that our European Groundshot Commission will help to direct the necessary attention to the concerning and significant impact that the conflict will have on cancer research, including but not limited to clinical trials in Europe. There is already a burgeoning east-west divide in European cancer research and it’s crucial the Russia-Ukraine war does not cause this gap to grow,” says Dr. Andreas Charalambous, President of the European Cancer Organisation.
The European Groundshot Commission also predicts that Brexit will continue to negatively impact European cancer research. The Commission analyzed data comparing EU28 (UK included) versus EU27 (UK not included) research activity and found a significant gap, one the Commission suggests is extremely unlikely to be bridged by increased research activity from the remaining EU27. Another key recommendation from the European Groundshot Commission is for European cancer research funders and the European cancer research community to mitigate the impact of Brexit and other political challenges by ensuring that the UK can continue to collaborate with European partners and contribute to European cancer research and innovation activities.
“UK cancer research in the post-Brexit world stands at a crossroads where strategic decisions will determine whether we continue to thrive and partner internationally or whether isolationism will reduce our world standing,” says Professor Richard Sullivan, co-lead for the Commission and Professor of Cancer & Global Health at Institute of Cancer Policy, King’s College London.
Professor Lawler adds, “If the UK is not involved in EU collaborative cancer research and not part of Horizon Europe’s research community, this will have an extremely detrimental effect on European cancer research activity. Ultimately, patients with cancer will the pay the price for this decision in terms of health-care outcomes.”
Gaps in European cancer research and its funding
The European Groundshot Commission analysis into investment in cancer research in Europe in 2010-19 found that the total amount of investment, excluding the private sector, was about 20-22 billion euros, about 26 euros per head. The minimum equivalent figure for the U.S. over the same period was 80.5 billion dollars (around 76 billion euros and 234 euros per head). Considering this dramatic gap in spending per head, the European Groundshot Commission calls for a doubling of the European cancer research budget to 50 euros per capita by 2030.
The European Groundshot Commission argues that cancer prevention research in particular has not had the funding it deserves. A greater focus on preventing cancer would reduce the number of people who develop cancer and therefore allow more resources to be available for those who do require treatment. The report calls for a significant reprioritization of cancer prevention, cancer screening, and early cancer detection research to reduce the burden of cancer for European citizens and enable those who do develop cancer access to more resources and the best treatments available.
“It is estimated that 40% of cancers in Europe could be prevented if primary prevention strategies made better use of our current understanding of cancer risk factors. There are already evidence-based and cost-effective cancer preventive interventions available, and we want to see more effective implementation and communication of these across Europe. Additionally, up to one-third of cancer cases in Europe are more likely to have a better outcome if they are detected early, but disappointingly, we find that rates of screening tests vary widely between different European countries. More research is needed to understand why people do not participate in cancer screening programs across Europe,” says Anna Schmutz, International Agency for Research on Cancer, France.
Gender equity in cancer research is another crucial gap identified in the European Groundshot Commission, with senior female authors making up less than a third of all authors for those European countries contributing the most cancer research outputs. The gender of principal investigators in Europe was also determined for 22, 291 cancer research projects: The majority of principal investigators were men with less than 33% women, reflecting the gender inequality that exists.
“Our data on female authors clearly illustrate the significant gender gap that exists in the European cancer research community. Greater research is needed into the reasons for why some European countries or regions have greater gender inequality in cancer research than others. Strategies based on these data would then hopefully improve the gender balance in cancer research in Europe,” says Professor Yolande Lievens, Ghent University Hospital, Ghent.
The Commissioners hope that the findings and recommendations in this report will help the European cancer research community as they work towards a more equitable agenda where all citizens and patients, no matter where they live, will benefit equally from advances in cancer research.
“This European Groundshot has a significant patient focus, which is very welcome,” said Teodora Kolarova, Bulgarian patient advocate and Executive Director of the International Neuroendocrine Cancer Alliance, “Too often the patient viewpoint is ignored, but it is front and center in this Commission. Patients need to be active participants in research, co-creating with their scientific and clinical colleagues. Another welcome focus is on central and eastern Europe—it is crucial that we see a critical upsurge in research in this region, so that the east-west divide is narrowed, not widened.”
Prof. Lawler adds, “Gathering data and turning them into cancer intelligence has been our North Star in this commission. Too often, opinion, even expert opinion, has trumped data in the genesis and implementation of cancer research policies. Simply continuing to dedicate resource and effort to a narrow research agenda is no longer desirable or viable: we must follow the data and act on what they reveal. We have an unrivaled opportunity to reimagine cancer research and its implementation so as to achieve our ambitious 70: 35 Vision, an average of 70% 10-year survival for patients treated for cancer in Europe by 2035. Let’s grasp this opportunity.”
Writing in a linked comment, Márcia Costa and David Collingridge, editors at The Lancet Oncology, say, “European leaders must break down the political barriers that divide the continent, rising above popularism, to work together in the common pursuit of harmonizing cancer research missions and national cancer plans, strengthening health systems, and supporting all patients with cancer, including those from neighboring countries in need of international aid. The research, data, recommendations, and actions summarized in the European Groundshot Commission could be powerful drivers of change if all actors are willing to listen and to put artificial divisions to one side. After all, we are all Europeans, irrespective of the politics, and we deserve better.”
More information:
European Groundshot—addressing Europe’s cancer research challenges: a Lancet Oncology Commission, The Lancet Oncology (2022). www.thelancet.com/commissions/ … shot-cancer-research
Journal information:
Lancet Oncology
Source: Read Full Article