When looking at the state of COVID-19 in the United States, Mansoor Amiji, distinguished professor in the Department of Pharmaceutical Sciences at Northeastern, invites you to think from the perspective of a virus. What does it want? What does it need to do to find new hosts, or to reinfect old ones?
The answer, he says, lies in spike proteins, the part of a virus that attaches to the receptor on a host cell. Under pressure from natural immunity and other countermeasures to its survival, the COVID-19 virus mutates these spike proteins at random, creating new variants that are more transmissible than previous ones.
This evolution makes COVID-19 similar to other viruses we’ve seen. “That’s really the natural course of a virus,” Amiji says.
It’s also the reason you’re more likely to get COVID-19 twice now than you were just four months ago. New variants like BA-4 or BA-5, which were unheard of earlier this year, are now circulating in the United States, and they may not be prevented by vaccines, boosters, or the antibodies that you develop when you’re infected by another variant.
For example, if you became infected from the BA-2 subvariant, this doesn’t prevent you from getting infected with BA-4 or BA-5, says Neil Maniar, professor of practice in the Department of Health Sciences. Maniar says each subvariant of COVID-19 tends to be more transmissible than the last, and that protection from one does not guarantee protection from another.
“It doesn’t mean that we have to fear reinfection,” Maniar says, “but it does mean we have to keep in mind that just because you got COVID once, it doesn’t mean you won’t get it again within a month or two months or three months, because there are these different subvariants that are circulating.”
Despite this development, the Centers for Disease Control and Prevention still does not recommend that you test for COVID-19 within 90 days of recovering from infection.
“If you tested positive for COVID-19 with a viral test within the previous 90 days and subsequently recovered and remain asymptomatic, you do not need to quarantine or get tested after close contact,” reads the CDC’s website.
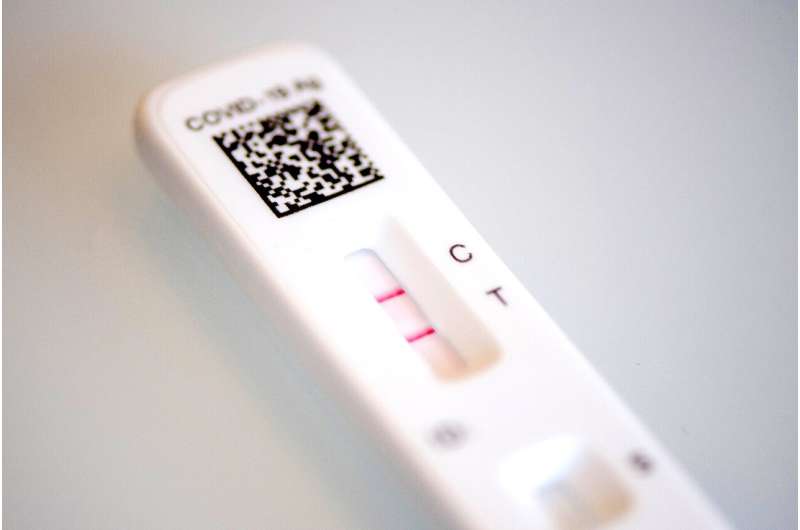
The reason for this, Maniar says, is that a PCR test can still detect trace amounts of the virus even after someone is no longer symptomatic or infectious. This can lead to a false positive, even when an antigen (or, “rapid”) test will come back negative.
“Those viral particles can be detected as far as two or three months out,” he says.
The thinking when the recommendation was written was also that the antibodies developed during the infection could protect you from getting reinfected within 90 days. But that’s not really the case, Maniar says.
“The idea that if you are infected, that you don’t necessarily have to worry about reinfection for three months, doesn’t necessarily apply anymore,” he says.
The return to the “new normal”—maskless workspaces and airplanes, for example—may increase the probability of reinfections from different variants.
“We’re really starting to return to a much more normal pace of life relative to earlier this year,” Maniar says. “That’s a really good thing.”
It means that we have resources at our disposal, like vaccines and masks, to gather in relative safety, he says. Still, “the likelihood of being exposed increases.”
Fortunately, as variants tend to become more infectious, they also tend to become less powerful. Amiji says COVID-19’s subvariants typically cause more upper respiratory issues than lower, making the symptoms less serious. And for those who have been vaccinated and received booster shots, symptoms tend to be even less severe, or even nonexistent. This reinforces the importance of getting vaccinated and boosted. Amiji hopes that one day COVID-19 boosters will combine with flu shots, and that it can be easy to get both at the same time each year.
But hospitalizations still happen, especially among subsets of the population that are at higher risk, so it is still important to take preventative measures even as we start to move into what Amiji calls an “endemic” phase of the pandemic.
To help stop the spread, Amiji recommends getting tested if you have symptoms, and if a rapid test—which is less sensitive than a PCR test—is positive, you should isolate and wear a mask indoors. The amount of time it takes to test negative after being infected varies from person to person, he says, but it’s important to keep testing in order to make informed decisions. “It’s the time when you start to test negative that you could potentially be less infective,” he says.
Source: Read Full Article
