Compared to other common supplemental screening methods, breast MRI was superior at detecting breast cancer in women with dense breasts, according to a study published in Radiology.
Breast cancer is one of the leading causes of cancer death in women. Roughly 47% of women in the United States have dense breasts, which is an independent risk factor of breast cancer. Women with dense breasts have a higher amount of glandular tissue and fibrous connective tissue and low amounts of fatty tissue in the breasts.
While screening mammography effectively detects up to 98% of cancer in fatty breasts, breast cancer is more easily missed in dense breasts. This results in a negative mammogram, giving patients false reassurance.
“Breast cancer masses appear white on a mammogram, and dense tissue also appears white, which makes finding breast cancers within dense breast tissue harder for radiologists,” said study co-author Vivianne Freitas, M.D., M.Sc., assistant professor at the University of Toronto, Canada, and staff radiologist at the Joint Department of Medical Imaging in Toronto.
Supplemental screening may be required to assist in cancer detection in women with dense breasts. The four most common supplemental imaging tests are hand-held breast ultrasound, automated breast ultrasound, digital breast tomosynthesis and breast MRI.
“Our study was designed to evaluate the role of different supplementary screening tests in women of average or intermediate risk of breast cancer with dense breast tissue who had a negative screening mammogram,” Dr. Freitas said.
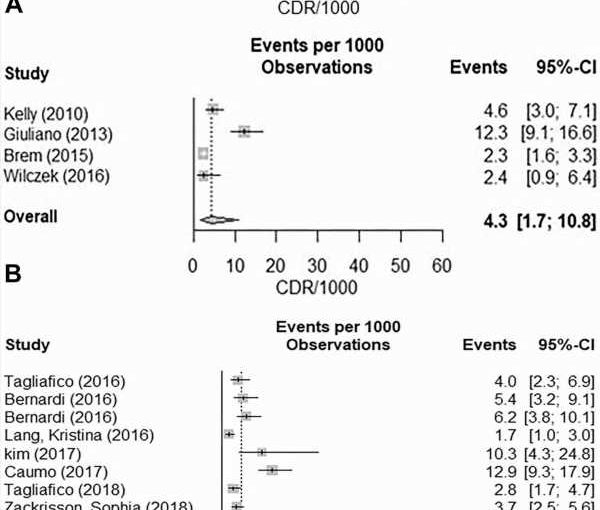
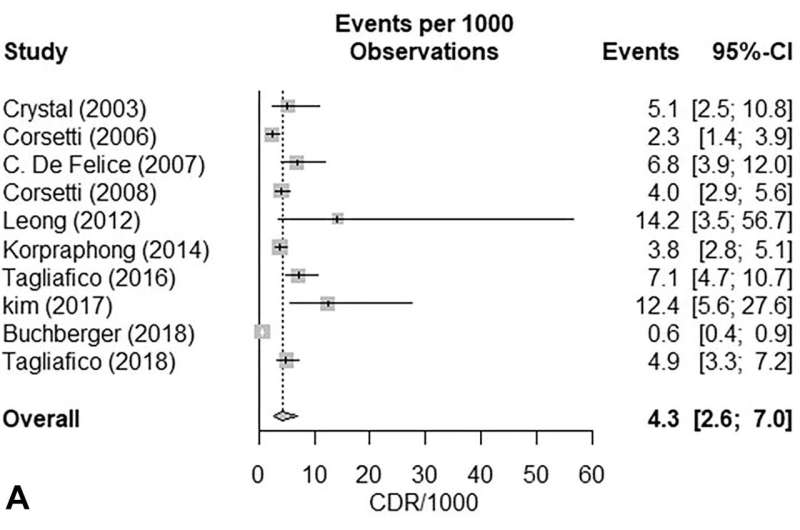
To measure which screening method was the most beneficial to women with dense breasts, researchers conducted a meta-analysis on 22 studies that included 261,233 patients screened for breast cancer. Ten of the studies covered hand-held breast ultrasound, four studies covered automated breast ultrasound, three studies covered breast MRI, and eight studies reported on digital breast tomosynthesis. Of the patients included, 132,166 patients had dense breasts and a negative mammogram.
Risk assessment models have been used to identify patients with an average and intermediate risk of developing breast cancer. In the United States, women with an estimated lifetime risk of 12 to 13% of developing breast cancer are considered average risk. Factors that elevate the risk to intermediate include having a history of treated breast cancer or previous breast biopsies with high-risk lesions. High-risk patients, with a lifetime risk of 20% or higher, were excluded from the study since the benefit of breast MRI is already established in high-risk populations.
Meta-analysis showed that of the 132,166 patients with dense breasts, a total of 541 breast cancers that were initially missed on mammography were detected with supplemental screening methods. Breast MRI was the superior screening method and was capable of detecting even the smallest of cancers. Excluding MRI, there was not a significant difference between the other supplemental screening methods.
“MRI is far superior in terms of cancer detection compared to hand-held ultrasound, automated ultrasound and digital breast tomosynthesis,” Dr. Freitas said. “Our results about the role of MRI in supplementary screening will allow stakeholders to guide healthcare policies in this setting and direct further research.”
While the results demonstrate the effectiveness of breast MRI in cancer detection, more research is needed.
“Before we can advocate for wider application of breast MRI in these women, further evaluation of cost-effectiveness of breast MRI compared to other techniques, effect on mortality reduction, etc., will need to be studied,” Dr. Freitas said. “At the current time, availability and cost of the breast MRI remain the biggest barrier for widespread implementation.”
More information:
Heba Hussein et al, Supplemental Breast Cancer Screening in Women with Dense Breasts and Negative Mammography: A Systematic Review and Meta-Analysis, Radiology (2023). DOI: 10.1148/radiol.221785
Journal information:
Radiology
Source: Read Full Article