Mount Sinai researchers have published one of the first studies to associate changes in blood gene expression during COVID-19 with the post-acute sequelae of SARS-CoV-2 infection, also known as “long COVID,” in patients more than a year after they were hospitalized with severe COVID-19.
The findings, published in Nature Medicine on December 8, highlight the need for greater attention at the infection stage to better understand how the processes that begin then eventually lead to long COVID, which could help improve both prevention strategies and treatment options for COVID-19 survivors experiencing persistent symptoms after infection.
The research team identified, among other findings, two molecularly distinct subsets of long COVID symptoms with opposing gene expression patterns during acute COVID-19 in plasma cells, the immune system’s antibody-producing cells. In patients who went on to develop lung problems, antibody production genes were less abundant.
However, for patients with other symptoms such as the loss of smell or taste and sleep disruptions, the same antibody production genes were more abundant instead. These opposing patterns observed in the same cells, as well as additional unique patterns observed in other cell types, point to the existence of multiple independent processes leading to different long COVID symptoms; these processes are already present during the acute infection.
“Our findings show that molecular processes leading to long COVID are already detectable during COVID-19 infection,” said senior author Noam D. Beckmann, Ph.D., Assistant Professor of Medicine (Data Driven and Digital Medicine) and Associate Director of Data Science Strategy at The Charles Bronfman Institute for Personalized Medicine at the Icahn School of Medicine at Mount Sinai.
“Furthermore, we see the start of multiple molecularly distinct paths leading to long COVID, providing a unique viewpoint into differences between long-term symptoms.”
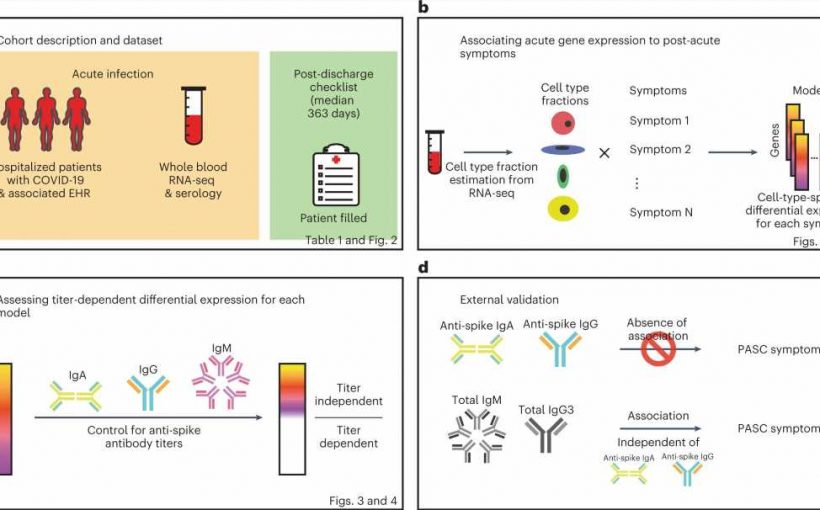
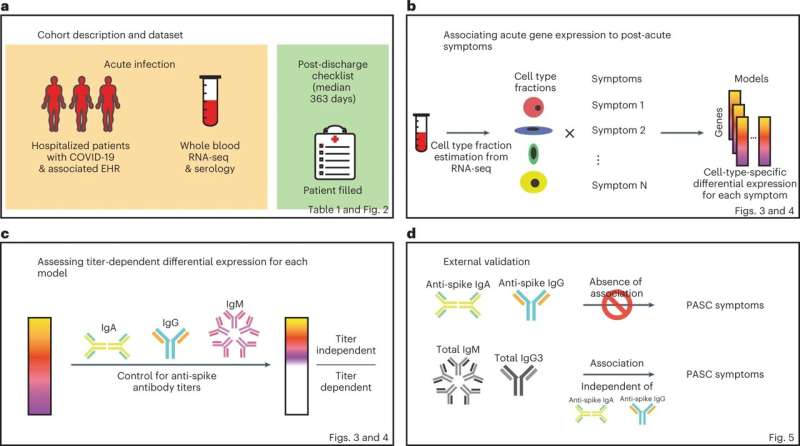
Using the Mount Sinai COVID-19 Biobank, the researchers examined gene expression data in blood samples from more than 500 patients hospitalized with COVID-19 between April and June 2020. More than 160 of these patients provided self-reported assessments of symptoms still present six months or more after hospitalization.
The team tested each gene expressed in the blood for association with each long COVID symptom, accounting for ICU admission, COVID-19 severity during hospitalization, sex, age, and other variables. The team then tested for associations specific to each of 13 different types of immune cells, including plasma cells. Finally, these associations were categorized by whether they matched up with changes in patients’ levels of antibodies specific to the virus.
“For long COVID symptoms, like smell or taste problems, connecting antibody gene expression in plasma cells with the actual levels of antibodies against the SARS-CoV-2 spike protein demonstrates a direct link to the body’s response to the virus,” said lead author Ryan C. Thompson, Ph.D., Data Science Analyst at The Charles Bronfman Institute for Personalized Medicine.
“On the other hand, the gene expression pattern for lung problems does not match up with SARS-CoV-2-specific antibody levels, highlighting the different immune processes leading to long COVID that are triggered by COVID-19.”
The team said long COVID still remains poorly defined and future studies should take the initial stage of infection into account to more comprehensively characterize the molecular processes of long COVID and identify biomarkers that can help predict, treat, and prevent prolonged symptoms.
“Our findings show there is the potential to use data from the infection stage to predict what might happen to the patient months later,” said co-corresponding author Alexander W. Charney, MD, Ph.D., Associate Professor of Genetics and Genomic Sciences, and Co-Director of The Charles Bronfman Institute for Personalized Medicine.
“We should not ignore the infection phase in research on long COVID—this is clearly a critical window of time where the body’s response to SARS-CoV-2 might be setting the stage for what is to come.”
More information:
Alexander Charney, Molecular states during acute COVID-19 reveal distinct etiologies of long-term sequelae, Nature Medicine (2022). DOI: 10.1038/s41591-022-02107-4. www.nature.com/articles/s41591-022-02107-4
Journal information:
Nature Medicine
Source: Read Full Article