When Emily Largent worked as an ICU nurse at UCLA, she didn’t shy away from the difficult cases. It wasn’t necessarily the medical procedures themselves that were challenging; caring for patients after organ transplants or managing a patient on life support were part of the job description. What really drew Largent to a case was the tough decisions that were involved. Should this patient really be a candidate for an organ transplant? What do we do when a patient’s family disagrees about ending life support?
As Largent worked on these cases, she saw the same questions come up again and again—and she had to solve them, again and again. “And it struck me,” she says, “that these might be instances where we need a systemic change, so that we weren’t repeatedly needing to come up with one-off solutions.”
That realization drove Largent to enter a bioethics fellowship at the National Institutes of Health (NIH) with Ezekiel Emmanuel, now a Penn Integrates Knowledge University Professor and the vice provost for global initiatives. She went on to obtain her J.D. and Ph.D. in health policy and is now an assistant professor of medical ethics and health policy at the University of Pennsylvania’s Perelman School of Medicine. While she no longer works in the ICU, she’s built a career dissecting the ethical issues around one of the leading causes of death in the United States: Alzheimer’s disease.
Alzheimer’s is “a huge public health problem,” says Largent. About 1 in 9 people older than 65 have Alzheimer’s dementia, and new diagnoses of the neurodegenerative disease are projected to double by 2050. The growing threat of Alzheimer’s has stoked the search for a cure or disease-modifying treatment.
With billions of dollars funneled into Alzheimer’s research each year, researchers have uncovered many of the molecular abnormalities underlying dementia and found new ways to test for risk factors and disease markers. This foundational research is essential to developing a cure, but it’s also revealed cracks in systems that exist to care for and protect patients with Alzheimer’s.
Using biomarkers for good
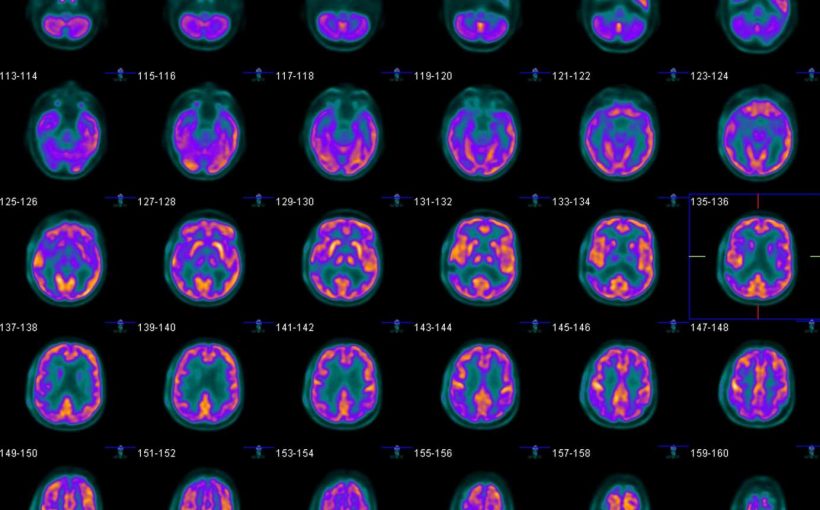
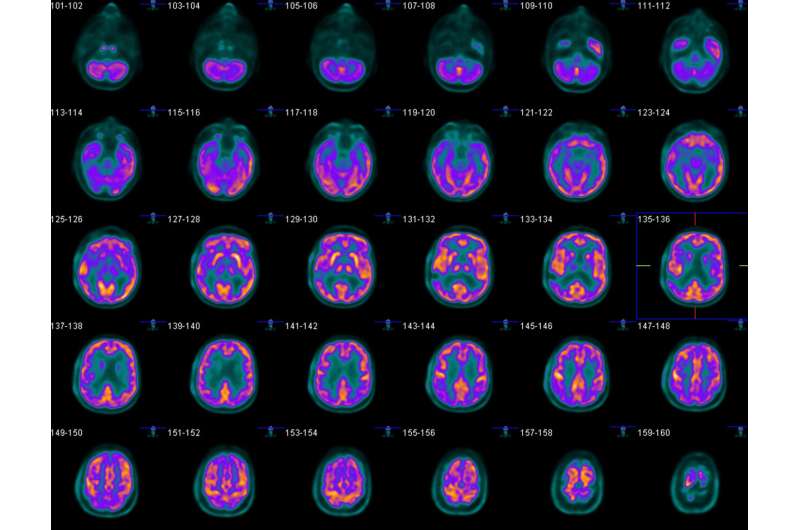
“Advances in research are changing what it means to have an Alzheimer’s diagnosis for both patients and their families,” Largent says. One of the ways that’s happening is through the use of biomarkers in research and in clinical practice. Biomarkers are physical indicators of a disease that can be measured through procedures like blood tests, imaging scans, or biopsies.
One of the most important biomarkers for Alzheimer’s is a protein called beta-amyloid. This protein makes up amyloid plaques, a brain abnormality that is a hallmark of Alzheimer’s disease. While amyloid plaques are most plentiful in the brains of patients with severe Alzheimer’s dementia, they begin accumulating long before patients notice any memory issues.
The fact that amyloid plaque buildup precedes memory loss has made the protein a prime target for researchers who want to study early-stage Alzheimer’s disease. Scientists believe that if a treatment is developed, it will work best if administered early, before Alzheimer’s has damaged the brain too extensively.
“There’s been a push in research studies to find people who have these biomarkers and are cognitively unimpaired,” Largent says. While having high amyloid levels doesn’t guarantee that a person will develop dementia down the line, it greatly increases the risk level. That makes people with high amyloid levels ideal candidates for clinical trials testing early interventions.
As the desire to find study participants with biomarkers for Alzheimer’s has grown, so, too, has the number of cognitively healthy people who are learning of their biomarker status. While amyloid tests have become an indispensable tool in research, Largent worries that disclosing biomarker status to unimpaired people—even if it comes with the possibility of medication to treat the disease—may have unforeseen consequences. “Socially, we’re not ready for this,” she says.
Her fears stem from the highly charged nature of biomarker results and their potential to turn a person’s life around. When Largent and her colleagues interviewed cognitively healthy individuals who had been diagnosed with high amyloid levels in a 2021 study published in the Journal of Law and the Biosciences, they found that for some the test results provoked feelings of disappointment and fear of losing their identity.
“A colonoscopy isn’t going to change who I am,” said one patient with elevated amyloid levels interviewed as part of the study. But “this is my brain involved.”
Largent’s research found that while a positive biomarker test result allowed patients to plan for the possibility of dementia, it also threatened their sense of self and cast a cloud over the coming years. These concerns didn’t go so far as to cause depression or suicidal thoughts, but they did shape who the patients told about their test results. Many with high amyloid levels worried how others would view them upon learning their Alzheimer’s risk status, even though they had no memory problems and may not develop any for years, if ever.
Those fears included a concern that employers, housing providers, and insurers learning of their biomarker status could lead to stigma and discrimination, and Largent agrees their anxieties are valid. “From where I sit, we have a situation where our scientific understanding of Alzheimer’s disease is rapidly outpacing any sort of existing law or policy protections,” she says. “We really don’t have legal protections for people who experience discrimination due to their biomarker status.”
‘Circles’ of influence
Earlier Alzheimer’s diagnoses don’t just affect the patient; they also change the lives of their spouse, families, and friends. Largent says that, when we consider the growing caseloads of Alzheimer’s, we also need to imagine the “circles” of people those cases affect. In a 2019 JAMA Neurology study, Largent found that early, biomarker-based diagnoses were causing those “circles” to grow. When a patient receives a test result with elevated amyloid or genetic risk factors, “you start to see people around them thinking about stepping into a caregiver role in the future,” Largent says.
That means more people are expecting to become informal or unpaid caregivers to Alzheimer’s and dementia patients in the coming years. “We have a huge over-reliance as a country on informal caregiving,” says Largent. It is a burden on many Americans that, according to the Centers for Disease Control, can lead to lost sleep, mental health issues, and even compromised physical health.
Caregivers can also play a large role in Alzheimer’s research itself. Alzheimer’s clinical trials often require a patient to enroll with a study partner, an individual close to the patient who can monitor the patient’s mental state, assist with daily tasks, administer medication, and ensure they come to their doctor’s visits.
When Largent examined who was most likely to step into a role as a study partner in a Journal of Alzheimer’s Disease study this year, she found that study partners were most often spouses. That means for Alzheimer’s patients without a spouse, enrolling in a clinical trial poses a bigger challenge.
“There’s a very good scientific and ethical rationale for requiring study partners,” says Largent, “but it can have these unintended consequences of disadvantaging some individuals who might want to enroll in research but aren’t able to.”
Caring solutions
Largent hopes that policies that regulate Alzheimer’s research will continue to develop so that patients who want to be part of clinical trials to find disease-modifying treatments can be included. She underscores the importance of providing resources and support to patients and caregivers and preparing for the demand on the health care system to grow.
Due to the growing popularity of biomarker use, Largent also advocates for legal protections for patients with early Alzheimer’s biomarkers and genetic risk factors, and she’s developing protocols that physicians can use to disclose patients’ biomarker test results in a responsible manner.
“I hope there’s a disease-modifying therapy we can give to people to slow or prevent the onset of dementia,” Largent says. But even if a new treatment is discovered, “We’re not going to have a solution for everyone. This is not a disease we’re going to just be able to cure our way out of. We’re going to have to do a lot of caring for people.”
More information:
Emily A. Largent et al, You’ve Got a Friend in Me: How Cognitively Unimpaired Older Adults Select a Study Partner to Participate with Them in Alzheimer’s Disease Research, Journal of Alzheimer’s Disease (2022). DOI: 10.3233/JAD-220061
Journal information:
Journal of Alzheimer’s Disease
,
Archives of Neurology
Source: Read Full Article