The proportion of people with current COVID-19 infection missed by the Innova lateral flow test (LFT) is substantial enough to be of clinical importance, particularly when testing people without symptoms, warn experts in The BMJ today.
An analysis by Professor Jonathan Deeks and colleagues predicts that Innova would miss 20% of viral culture positive cases attending an NHS Test-and-Trace center, 29% without symptoms attending mass testing, and 81% attending university screen testing without symptoms—many more than predicted by mathematical models on which policy decisions are based.
The authors acknowledge that LFTs are an important tool in controlling the COVID-19 pandemic, but say claims that LFTs can identify “the vast majority who are infectious” have been overstated, with risk of false reassurance to those seeking to rule-out infection.
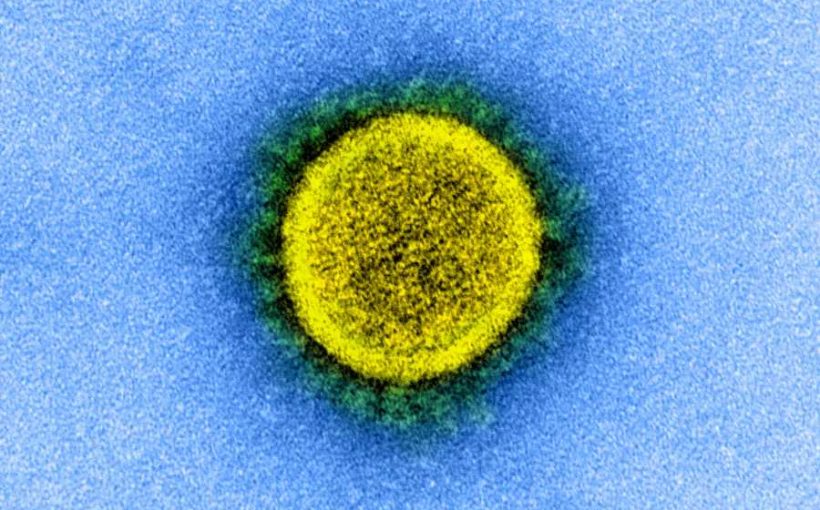
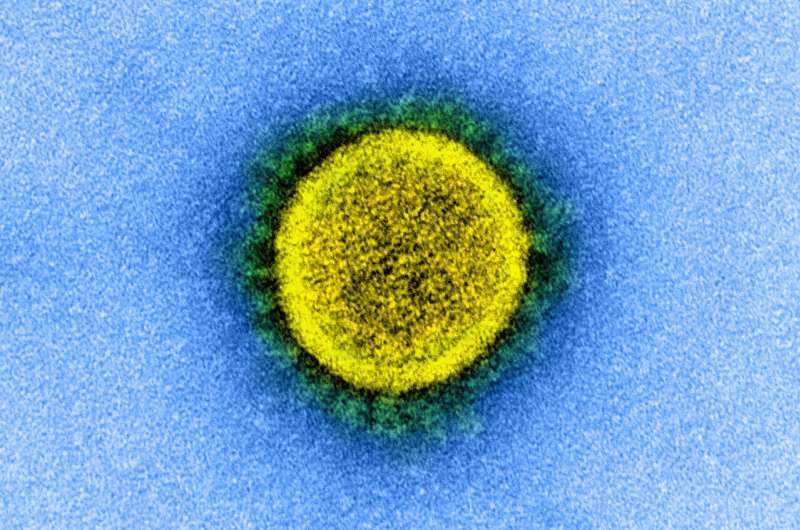
Lateral flow tests (LFTs) for SARS-CoV-2 (the virus responsible for COVID-19) have been recommended for widespread use, largely based on predictions made by mathematical models.
While empirical data show LFTs give a positive result when virus is present on a swab in high quantities, and therefore can detect people who are likely to be infectious, the proportion missed who are infectious has not been evaluated.
To address this evidence gap, Deeks and colleagues drew on empirical data from several sources to predict the proportion of Innova LFTs that produce negative results in those with a high risk of SARS-CoV-2 infectiousness. They then compared these with predictions made by influential mathematical models.
Their focus was to identify the joint probability that people are likely to be infectious (in that they have a viral culture positive result or are a secondary case) and that they test negative on Innova.
Their results are based on testing in three settings: symptomatic testing at an NHS Test-and-Trace center, mass testing in Liverpool in residents without symptoms, and in students at the University of Birmingham.
The analysis predicted that of those with a viral culture positive result, Innova would miss 20% attending an NHS Test-and-Trace center, 29% without symptoms attending municipal mass testing, and 81% attending university screen testing without symptoms, along with 38%, 47%, and 90% of sources of secondary cases.
In comparison, two mathematical models underestimated the numbers of missed infectious individuals (8%, 10%, and 32% in the three settings for one model, whereas the assumptions from the second model made it impossible to miss an infectious individual).
The authors stress that evaluating the accuracy of a test for current infection or infectiousness is challenging owing to the lack of a reference standard, and say there is the potential for error in their estimates. “The findings in this analysis therefore must be taken as illustrative and not exact,” they say.
However, they point out that these data “are currently the best available and clearly show that missing people with current infection or who are infectious is possible in all settings.”
“Allowing for the uncertainties in the results from our analyses, the proportion of people with current infection missed by the Innova LFT is likely to be of public health importance, particularly in settings with greater proportions of infectious people with lower viral loads; where the tests are often being applied,” they write.
They argue that key models have failed to appropriately use empirical evidence to inform assumptions of test accuracy and chances of infectiousness, resulting in unrealistic overestimates of test performance, and say until new generation LFTs are available that meet the regulatory performance requirements, negative test results from LFTs cannot be relied on to exclude current infection.
“Policy makers need to ensure that the public are aware of the risk of being infectious despite testing negative, and that tests are not used in situations where the consequences of false negative results are considerable,” they conclude.
When rapid antigen tests were introduced, we were promised they would “identify those who are likely to spread the disease, and when used systematically in mass testing could reduce transmissions by 90%.” Yet despite the UK spending more than £7bn on lateral flow devices since mid-2020, the lack of hard evidence on this promised impact is striking, argue public health experts in a linked opinion article.
They point out that observational studies attempting to assess the impact on transmission as a result of testing asymptomatic non-contacts have struggled to show an effect and none seem to have examined the costs of the programs.
Meanwhile, the World Health Organization cautions against mass asymptomatic testing because of high costs, lack of evidence on the impact, and risk of diverting resources from more important activities.
Source: Read Full Article