CAR T cell therapy is a promising immunological treatment for cancer. It involves the engineering chimeric antigen receptors (CAR) to redirect T cells towards targeted cancer cells.
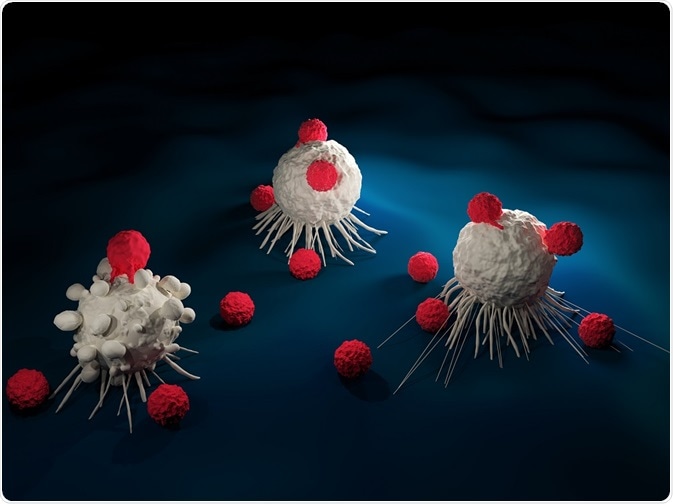
Credit: Meletios Verras/Shutterstock.com
Clinical efficacy of this technique to treat hematologic malignancies has been proved and ongoing studies are investigating its role to treat solid tumors. CAR T cells can also be applied to manage side effects, including cytokine release syndrome.
CAR T cell therapy for hematologic malignancies
CAR T cell therapy has proved successful in clinical trials to treat hematologic malignancies. The targeting of CD19, a surface antigen expressed on precursor and mature B cells, can treat B cell malignancies, such as chronic lymphocytic leukemia and non-Hodgkin lymphoma.
In 2017, the FDA approved two CAR T cell therapies for the treatment of acute lymphoblastic leukemia in children and adult advanced lymphomas.
Multiple myeloma is a hematologic malignancy of plasma cells with a high fatality rate. It requires novel treatment strategies, and current drugs and regimens for multiple myeloma are not curative for majority of patients with the disease.
Although the cells of multiple myeloma do not routinely express detectable CD19, CAR T cell therapy may be employed to target progenitor cells which are B cell in origin. A successful trial used CAR T cells as a salvage therapy for multiple myeloma patients who had received previous treatments. After 12 months, the patients had no laboratory evidence or clinical signs of the cancer indicating that CAR T cell therapy may be a valid treatment for the disease.
CAR T cell therapy for solid tumors
CAR T cells have the potential to provide novel treatments for solid tumors, but clinical trials have proved less successful than those for blood cancer therapy. Barriers to successfully treat solid tumors through CAR T cell therapy include cell surface antigen heterogeneity and the immunosuppressive microenvironment of tumors.
Cell surface antigen heterogeneity prevents a successful response in solid tumors because CAR T cell therapy relies on the specific targeting of single antigens. Clinical response is therefore reduced in solid tumors that display variation in antigen expression.
Future developments will involve simultaneously targeting multiple tumor antigens may lead to better cell coverage and improved treatments. Though recent studies show improved response to dual targeted CAR T cells, there is a possibility of developing resistance to the treatment with previous evidence indicating some selection for clonal variants resistant to treatment.
In comparison to certain blood cancers, solid tumors do not contain conventional co-stimulatory molecules that aid CAR T cell therapy and are able to actively suppress the immune system through various immunosuppressive pathways. This includes production of transforming growth factor beta (TGFβ), an inhibitor of T cell activation and proliferation.
The tumor microenvironment is also characterized by increased inflammatory activity that creates reactive oxygen species known to reduce antitumor response. Countermeasures have been proposed to overcome such inhibitory effects and increase the success of CAR T cell activity in solid tumors. The employment of immunostimulatory cytokines that block tumor-associated inhibition is one such strategy and early studies show improved clinical efficacy.
Managing toxicity in CAR T cell therapy
Future applications of CAR T cell therapy require enhanced management of side effects. Cytokine release syndrome is a serious side effect of CAR T cell therapy caused by the large and rapid release of cytokines from immune cells. The increased amounts of cytokines in the bloodstream can cause symptoms, including fever, a rapid heartbeat, and difficulty in breathing.
Cytokine release syndrome is an expected outcome of CAR T cells being active in the body during treatment and must be managed through standard support therapies. Though CAR T cell therapy can decrease the toxicity of treatment associated with conventional cancer therapy, the severe-immune mediated adverse reactions show long term persistence up to 10 years in clinical trials. Thus, managing potential long term side effects is an important factor for future CAR T cell therapy applications.
Sources:
- National Cancer Institute: CAR T Cells: Engineering Patients’ Immune Cells to Treat Their Cancers
- Ghosh, A. et al. 2017. CAR T cell therapy for multiple myeloma: where are we now and where are we headed? Leukemia & Lymphoma, 6, pp. 1-12.
- Mirzaei, H.R. et al. 2017. Chimeric Antigen Receptors T Cell Therapy in Solid Tumor: Challenges and Clinical Applications, Frontiers in Immunology, 8, e1850.
- Bonifant, C.L. et al. 2016. Toxicity and management in CAR T-cell therapy, Molecular Therapy Oncolytics, 3: 16011.
Further Reading
- All Oncology Content
- What is Oncology?
- Oncology Therapy
- Oncology Palliative Care
- Oncology Ethical Issues
Last Updated: Aug 24, 2018

Written by
Shelley Farrar Stoakes
Shelley has a Master's degree in Human Evolution from the University of Liverpool and is currently working on her Ph.D, researching comparative primate and human skeletal anatomy. She is passionate about science communication with a particular focus on reporting the latest science news and discoveries to a broad audience. Outside of her research and science writing, Shelley enjoys reading, discovering new bands in her home city and going on long dog walks.
Source: Read Full Article
